Associations between sleep duration, sleep quality and high sensitivity C-reactive protein among medical students of a medical college in Chhattisgarh, India
Abstract
Background: Recent studies in human have indicated possible pathophysiologic mechanisms to support the biologic plausibility of an association between sleep deprivation and future cardiovascular risk. In addition, emerging evidence suggests that inflammatory markers are elevated in sleep-deprived individuals. However, the relationship between sleep duration and inflammatory markers is still unclear.The aim of this study was to investigate associations between self-reported sleep duration, sleep quality, and high sensitivity C-reactive protein (hs-CRP) levels among medical students of a medical college in Chhattisgarh, India.
Materials and Methods: A total of 150 Students (94 male, 56 female) of Government Medical College, Rajnandgaon, Chhattisgarh in the age group of 20 to 30 years were randomly enrolled in the present study. Blood samples were analyzed for fasting blood glucose and hs-CRP. Sleep duration and sleep quality was assessed using the Pittsburgh Sleep Quality Index (PSQI).
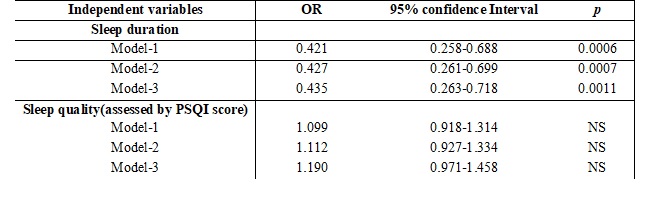
Results: In the present study, a significant variation in serum hs-CRP levels with different sleep categories was observed (P<0.0001), with the hs-CRP levels being highest (Mean ± SD; 1.13±0.85 mg/L) in short duration (<6 hours) followed by long duration (>8hours) sleepers (Mean± SD; 0.79±0.41mg/L). In both linear and logistic regression analysis model adjusted for various risk factors for cardiovascular disease, short sleep duration was significantly associated with elevated serum hs-CRP levels.
Conclusion: Our findings suggest that in¬flammatory mechanisms may play a role in the cardiovascular risk associated with sleep deprivation.
Downloads
References
Watson NF, Badr MS, Belenky G, et al. Recommended amount of sleep for a healthy adult: a joint consensus statement of the American academy of sleep medicine and sleep research society. Sleep. 2015 Jun 1;38(6):843-4. doi: https://doi.org/10.5665/sleep.4716.
Spiegel K, Leproult R, Van Cauter E. Impact of sleep debt on metabolic and endocrine function. Lancet. 1999 Oct 23;354(9188):1435-9. DOI: https://doi.org/10.1016/S0140-6736(99)01376-8.
Insufficient sleep is a public health problem. CDC features: data and statistics 2015. Available from: http://www.cdc.gov/features/dssleep.
Wong JG, Patil NG, Beh SL, et al. Cultivating psychological well-being in Hong Kong's future doctors. Med Teach. 2005 Dec;27(8):715-9. DOI: https://doi.org/10.1080/01421590500237945.
Miller MA, Cappuccio FP. Inflammation, sleep, obesity and cardiovascular disease. Curr Vasc Pharmacol. 2007 Apr;5(2):93-102.
Shearer WT, Reuben JM, Mullington JM, et al. Soluble TNF-alpha receptor 1 and IL-6 plasma levels in humans subjected to the sleep deprivation model of spaceflight. J Allergy Clin Immunol. 2001 Jan;107(1):165-70.
Gabay C, Kushner I. Acute-phase proteins and other systemic responses to inflammation. N Engl J Med. 1999 Feb 11;340(6):448-54. DOI: https://doi.org/10.1056/NEJM199902113400607.
Ridker PM. High-sensitivity C-reactive protein and cardiovascular risk: rationale for screening and primary prevention. Am J Cardiol. 2003 Aug 21;92(4B):17K-22K.
Lagrand WK, Visser CA, Hermens WT, et al. C-reactive protein as a cardiovascular risk factor: more than an epiphenomenon? Circulation. 1999 Jul 6;100(1):96-102.
Pasceri V, Willerson JT, Yeh ET. Direct proinflammatory effect of C-reactive protein on human endothelial cells. Circulation. 2000 Oct 31;102(18):2165-8.
Chiang JK. Short duration of sleep is associated with elevated high-sensitivity C-reactive protein level in Taiwanese adults: a cross-sectional study. J Clin Sleep Med. 2014 Jul 15; 10(7):743-9. doi: https://doi.org/10.5664/jcsm.3862.
Ferrie JE, Kivimäki M, Akbaraly TN, et al. Associations between change in sleep duration and inflammation: Findings on C - reactive protein and Interleukin 6 in the Whitehall II Study. Am J Epidemiol. 2013; 178(6): 956–61. doi: https://doi.org/10.1093/aje/kwt072. Epub 2013 Jun 25.
Hall MH, Lee L, Matthews KA. Sleep duration during the school week is associated with C-reactive protein Risk Groups in healthy adolescents.Sleep Med. 2015; 16(1): 73–78. doi: https://doi.org/10.1016/j.sleep.2014.10.005. Epub 2014 Oct 28.
Nakamura K, Sakurai M, Miura K, et al. Overall sleep status and high sensitivity C-reactive protein: a prospective study in Japanese factory workers. J Sleep Res. 2014 Dec;23(6):717-727. doi: https://doi.org/10.1111/jsr.12182. Epub 2014 Aug 2.
Baessler A, Nadeem R, Harvey M, et al. Treatment for sleep apnea by continuous positive airway pressure improves levels of inflammatory markers - a meta-analysis. J Inflamm(Lond). 2013 Mar 22;10:13. doi: https://doi.org/10.1186/1476-9255-10-13. eCollection 2013.
Buysse DJ, Reynolds CF 3rd, Monk TH, et al. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989 May;28(2):193-213.
Meier-Ewert HK, Ridker PM, Rifai N, et al. Effect of sleep loss on C-reactive protein, an inflammatory marker of cardiovascular risk. J Am Coll Cardiol. 2004 Feb 18;43(4):678-83.DOI: https://doi.org/10.1016/j.jacc.2003.07.050.
Dowd JB, Goldman N, Weinstein M. Sleep duration, sleep quality, and biomarkers of inflammation in a Taiwanese population. Ann Epidemiol. 2011 Nov;21(11):799-806. doi: https://doi.org/10.1016/j.annepidem.2011.07.004. Epub 2011 Sep 1.
Taheri S, Austin D, Lin L, et al. Correlates of serum C-reactive protein (CRP)--no association with sleep duration or sleep disordered breathing. Sleep. 2007 Aug;30(8):991-6.
Miller MA, Kandala NB, Kivimaki M, et al. Gender differences in the cross-sectional relationships between sleep duration and markers of inflammation: Whitehall II study. Sleep. 2009 Jul;32(7):857-64.
Parthasarathy S, Vasquez MM, Halonen M et al. Persistent insomnia is associated with mortality risk. Am J Med. 2015 Mar;128(3):268-75.e2. doi: https://doi.org/10.1016/j.amjmed.2014.10.015. Epub 2014 Oct 16.
Everson CA. Clinical assessment of blood leukocytes, serum cytokines, and serum immunoglobulins as responses to sleep deprivation in laboratory rats. Am J Physiol Regul Integr Comp Physiol. 2005 Oct;289(4):R1054-63. Epub 2005 Jun 9.
Donga E, van Dijk M, van Dijk JG, et al. A single night of partial sleep deprivation induces insulin resistance in multiple metabolic pathways in healthy subjects. J Clin Endocrinol Metab. 2010 Jun;95(6):2963-8. doi: https://doi.org/10.1210/jc.2009-2430. Epub 2010 Apr 6.
Faraut B, Nakib S, Drogou C, et al. Napping reverses the salivary interleukin-6 and urinary norepinephrine changes induced by sleep restriction. J Clin Endocrinol Metab. 2015 Mar;100(3):E416-26. doi: https://doi.org/10.1210/jc.2014-2566. Epub 2015 Feb 10.
Van Leeuwen WM, Lehto M, Karisola P, et al. Sleep restriction increases the risk of developing cardiovascular diseases by augmenting proinflammatory responses through IL-17 and CRP. PLoS One. 2009;4(2):e4589. doi: https://dx.doi.org/10.1371%2Fjournal.pone.0004589. Epub 2009 Feb 25.
Irwin M, Thompson J, Miller C, et al. Effects of sleep and sleep deprivation on catecholamine and interleukin-2 levels in humans: clinical implications. J Clin Endocrinol Metab. 1999 Jun;84(6):1979-85.DOI: https://doi.org/10.1210/jcem.84.6.5788.
Irwin MR, Wang M, Ribeiro D, et al. Sleep loss activates cellular inflammatory signaling. Biol Psychiatry. 2008 Sep 15;64(6):538-40. doi: https://doi.org/10.1016/j.biopsych.2008.05.004. Epub 2008 Jun 17.
Richardson MR, Churilla JR. Sleep Duration and C-Reactive Protein in US Adults. South Med J. 2017 Apr;110(4):314-317. doi: https://doi.org/10.14423/smj.0000000000000632.
Huang WY, Huang CC, Chang CC, et al. Associations of self-reported sleep quality with circulating interferon gamma-inducible protein 10, interleukin 6, and high-sensitivity C-reactive protein in healthy menopausal women. PLoS One. 2017 Jan 6;12(1):e0169216. doi: https://dx.doi.org/10.1371%2Fjournal.pone.0169216. eCollection 2017.
Knutson KL. Does inadequate sleep play a role in vulnerability to obesity? Am J Hum Biol. 2012 May-Jun;24(3):361-71. doi: https://doi.org/10.1002/ajhb.22219. Epub 2012 Jan 24.
Patel SR, Hu FB. Short sleep duration and weight gain: a systematic review. Obesity (Silver Spring). 2008 Mar;16(3):643-53. doi: https://doi.org/10.1038/oby.2007.118. Epub 2008 Jan 17.
Spiegel K, Leproult R, L'hermite-Balériaux M, et al. Leptin levels are dependent on sleep duration: relationships with sympathovagal balance, carbohydrate regulation, cortisol, and thyrotropin. J Clin Endocrinol Metab. 2004 Nov;89(11):5762-71.DOI: https://doi.org/10.1210/jc.2004-1003.
Dettoni JL, Consolim-Colombo FM, Drager LF, et al. Cardiovascular effects of partial sleep deprivation in healthy volunteers. J ApplPhysiol (1985). 2012 Jul;113(2):232-6. doi: https://doi.org/10.1152/japplphysiol.01604.2011. Epub 2012 Apr 26.
Sgoifo A, Buwalda B, Roos M, et al. Effects of sleep deprivation on cardiac autonomic and pituitary-adrenocortical stress reactivity in rats. Psychoneuroendocrinology. 2006 Feb;31(2):197-208. Epub 2005 Sep 12.DOI: https://doi.org/10.1016/j.psyneuen.2005.06.009.
Takase B, Akima T, Satomura K, et al. Effects of chronic sleep deprivation on autonomic activity by examining heart rate variability, plasma catecholamine, and intracellular magnesium levels. Biomed Pharmacother. 2004 Oct;58 Suppl1:S35-9.
Zhong X, Hilton HJ, Gates GJ, et al. Increased sympathetic and decreased parasympathetic cardiovascular modulation in normal humans with acute sleep deprivation. J Appl Physiol (1985). 2005 Jun;98(6):2024-32. Epub 2005 Feb 17.
Azad MC, Fraser K, Rumana N,et al. Sleep Disturbances among Medical Students: A Global Perspective. J Clin Sleep Med. 2015 Jan 15;11(1):69-74. doi: https://dx.doi.org/10.5664%2Fjcsm.4370.
Bahammam AS, Al-Khairy OK, Al-Taweel AA. Sleep habits and patterns among medical students. Neurosciences (Riyadh). 2005 Apr;10(2):159-62.
Spira AP, Beaudreau SA, Stone KL, et al. Reliability and validity of the Pittsburgh Sleep Quality Index and the Epworth Sleepiness Scale in older men. J Gerontol A Biol Sci Med Sci. 2012 Apr;67(4):433-9. doi: https://doi.org/10.1093/gerona/glr172. Epub 2011 Sep 20.
Backhaus J, Junghanns K, Broocks A, et al. Test-retest reliability and validity of the Pittsburgh Sleep Quality Index in primary insomnia. J Psychosom Res. 2002 Sep;53(3):737-40.
Mollayeva T, Thurairajah P, Burton K, et al. The Pittsburgh sleep quality index as a screening tool for sleep dysfunction in clinical and non-clinical samples: A systematic review and meta-analysis. Sleep Med Rev. 2016 Feb;25:52-73. doi: https://doi.org/10.1016/j.smrv.2015.01.009. Epub 2015 Feb 17.


 OAI - Open Archives Initiative
OAI - Open Archives Initiative


