Pulmonary and Extrapulmonary Tuberculosis, An Inflammatory Disease Misdiagnosed as Cancer
Gheryani NA1*, Elkwafi RS2, Anbaig A3, Berras Ali RJ4, Elmatri H5
DOI:https://doi.org/10.17511/ijmrr.2024.i03.01
1* Nabeia Al Gheryani, Department of Pathology, Faculty of Medicine, University of Benghazi, Benghazi, Libya.
2 Raja S Elkwafi, Department of Pathology, Faculty of Medicine, University of Benghazi, Benghazi, Libya.
3 Amal Anbaig, Department of Pathology, Faculty of Medicine, University of Benghazi, Benghazi, Libya.
4 Rasheed J Berras Ali, Faculty of Medicine, University of Benghazi, Benghazi, Libya.
5 Haitham Elmatri, Department of Otolaryngology, Hospital of Benghazi, Benghazi, Libya.
Introduction: Tuberculosis is a serious infection associated with a high mortality rate if not treated. The clinical and imaging presentation are usually nonspecific and can mimic malignancy; therefore, extrapulmonary TB should be considered in the differential diagnosis of any suspicious extrapulmonary masses, particularly in immunocompromised patients.
Objective: This study aims to analyse 160 cases of pulmonary and extra-pulmonary tuberculosis correlate the pathological features with the clinical data and find the most common differentiation diagnosis of both pulmonary and extrapulmonary tuberculosis.
Methodology: A retrospective analysis of 160 cases of pulmonary and extra-pulmonary tuberculosis was performed. The age, gender, site, and symptoms of the lesion were collected, extrapulmonary sites were detected including rare and unusual sites and the differential diagnosis of these lesions was highlighted. The data were plotted in graphs and were analyzed.
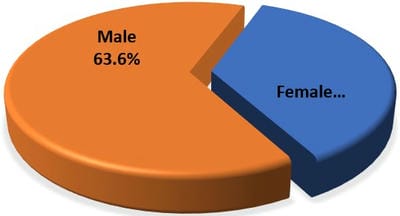
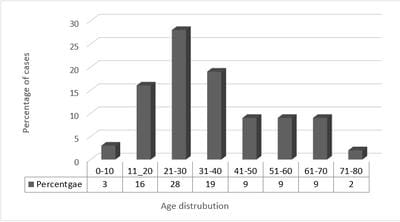
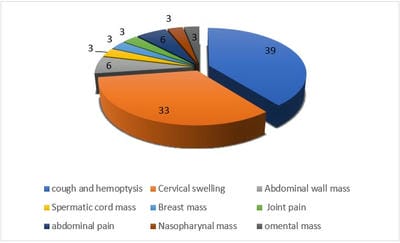
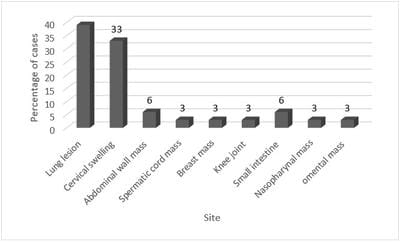
Result: In our study 63.6% were male and 36.4 were females. The majority of the patients were in the age group of 21-30 years followed by 31- 40 years, cough and hemoptysis were the most common symptoms followed by cervical swelling with 39% and 33% respectively. The most common sites were lung with (39%) and cervical swelling with (33%). The main differential diagnosis for many pulmonary and all extra-pulmonary tuberculosis was malignancy.
Conclusion: Tuberculosis is a serious young person's disease that can affect almost every organ and tissue of the body and should be considered in the differential diagnosis of suspicious masses, as tuberculosis is often misdiagnosed as cancer.
Keywords: Mycobacterium Tuberculosis, Cancer, Malignancy, Extrapulmonary
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Department of Pathology, Faculty of Medicine, University of Benghazi, Benghazi, , Libya. Email: |
Gheryani NA, Elkwafi RS, Anbaig A, Berras Ali RJ, Elmatri H, Pulmonary and Extrapulmonary Tuberculosis, An Inflammatory Disease Misdiagnosed as Cancer. Int J Med Res Rev. 2024;10(3):65-71. Available From https://ijmrr.medresearch.in/index.php/ijmrr/article/view/1473 |


 ©
©