Prevalence of Bronchogenic carcinoma in the North Indian Population
Pandey S.1, Mishra A.2, Chawla K.3, Kumar Shukla R.4*
DOI: https://doi.org/10.17511/ijmrr.2021.i05.05
1 Sanjay Pandey, Senior Consultant, Department of Surgery, District Female Hospital, Mirzapur, Uttar Pradesh, India.
2 Archana Mishra, Assistant Professor, Department of Biochemistry, MLN Medical College, Prayagraj, Uttar Pradesh, India.
3 Kavita Chawla, Professor, Department of Physiology, Moti Lal Nehru Medical College, Prayagraj, Uttar Pradesh, India.
4* Rakesh Kumar Shukla, Assistant Professor, Department of Anatomy, Autonomous State Medical College and Hospital, Mirzapur, Uttar Pradesh, India.
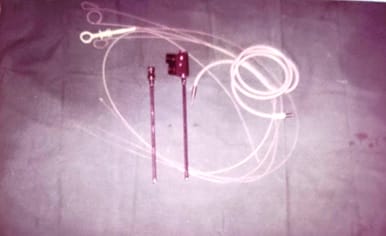
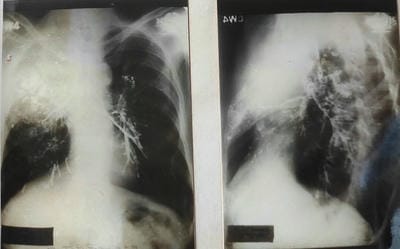
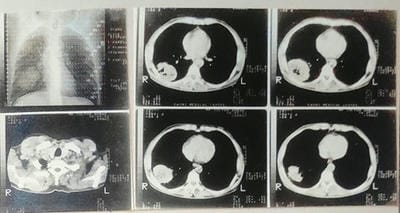
Aim: This original research article aims to study the Prevalence of Bronchogenic carcinoma in the North Indian Population. Material & Method: The present study includes 150 patients with intrathoracic space-occupying lesions, of which 42 patients with bronchogenic carcinoma were seen at SS hospital Banaras Hindu University, Varanasi, UP. Most of the patients studied were from the thoracic surgery section, while few patients were taken from other departments of SS hospital. The age of those patients varied widely, starting from 10 years to 60 years. During this study, patients were investigated in systemic order with the progression of symptoms from the onset, development of latest symptoms and treatment taken before if any, history of tuberculosis, chronic cough, smoking, and contact with were recorded. Result: Maximum patients were in the age group of 41 to 50 years. Forty-two patients were diagnosed with Bronchogenic carcinoma, a definitive diagnosis was confirmed by Clinical & Radiological (chest X-ray & CT Scan) in 24 (16%), by Bronchoscopic examination & Biopsy in 15 (10%) and by thoracotomy in 03(2%). The maximum age group among the cases were 41-60. The most common symptom was Cough with expectoration in 33 patients (78.5%), followed by Haemoptysis and Dyspnea in 30 cases (71.4%). Fever was least common with 6 cases. It was observed that 18 patients (43%) had the habit of smoking for more than 18 years. Conclusion: This study provides a framework for assessing the prevalence of bronchogenic carcinoma in the North Indian population and proves that smoking is a potential risk factor in bronchogenic carcinoma. Prevalence of Bronchogenic Carcinoma among all cases of Intrathoracic Lesions Cases 28 % and among all subjects who undergone for screening in one year – 2.84%.
Keywords: Epidemiology, India, Lung Cancer, Nonsmokers, Smokers, Lung Cancer Diagnosis, Bronchogenic Carcinoma
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Assistant Professor, Department of Anatomy, Autonomous State Medical College and Hospital, Mirzapur, Uttar Pradesh, India. Email: |
Sanjay Pandey, Archana Mishra, Kavita Chawla, Rakesh Kumar Shukla, Prevalence of Bronchogenic carcinoma in the North Indian Population. Int J Med Res Rev. 2021;9(5):306-314. Available From https://ijmrr.medresearch.in/index.php/ijmrr/article/view/1333 |


 ©
©