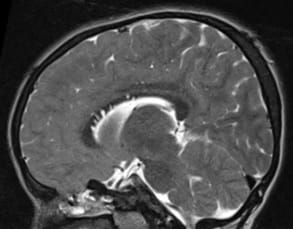
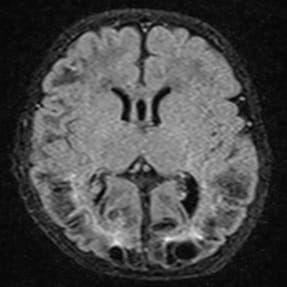
Etiological classification of seizures in pediatric age group (6-12years) – MRI study
Gopalakrishnan N.1, Gaffoor M.2*
DOI: https://doi.org/10.17511/ijmrr.2021.i04.08
1 Nirmalkumar Gopalakrishnan, Associate Professor, Sri Venkateshwaraa Medical College Hospital and Research Centre, Puducherry, India.
2* Mohammed Ansari Gaffoor, Assistant Professor, Sri Venkateshwaraa Medical College Hospital and Research Centre, Puducherry, India.
Background: A seizure is an occurrence of signs or symptoms due to abnormal excessive or synchronous neuronal activity in the brain. The present study aims to study the etiological factors and clinical profile for new-onset seizures in children aged 6-12 years and to determine the frequency of Magnetic resonance imaging (MRI) abnormalities in the pediatrics age group with new-onset unprovoked seizure and those with inadequately investigated longstanding epilepsy and classify the etiology based on the MRI findings. Methods: A prospective study involving a total of 50 patients was recruited aged between 6 to 12 years. All of them underwent neuro-imaging with MRI. Uncooperative patients were imaged following sedation and monitoring by the anesthetist. All children aged 6-12 years who presented with new-onset seizures were included. All MR images were obtained at a 3-mm section thickness except magnetization-prepared rapid gradient-echo images, which are obtained at a 1.8-mm section thickness. Results: Of the 50 patients 28 presented with generalized tonic-clonic seizures, 12 with simple partial seizures, 10 with complex partial seizures. Generalized seizures were a more common presentation than partial seizures in children 6-12 years of age. Conclusion: With the positivity of the MRI in the new-onset seizure in children between 6-12 years in our study gives an important aspect of the essential factor of imaging in pediatric new-onset seizures.
Keywords: Seizures, Children, MRI
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Assistant Professor, Sri Venkateshwaraa Medical College Hospital and Research Centre, Puducherry, India. Email: |
Gopalakrishnan N, Gaffoor A. Etiological classification of seizures in pediatric age group (6-12years) – MRI study. Int J Med Res Rev. 2021;9(4):257-262. Available From https://ijmrr.medresearch.in/index.php/ijmrr/article/view/1316 |


 ©
©