Evaluation of spectrum of MRI findings in children with Hypoxic Ischemic Encephalopathy and its comparison with transcranial sonography
Mathur M.1, Gupta I.2*, Mittal D.3
DOI: https://doi.org/10.17511/ijmrr.2021.i02.06
1 Manoj Mathur, Professor, Department of Radiodiagnosis, Govt. Medical College and Rajindra Hospital, Patiala, Punjab, India.
2* Ishita Gupta, Junior Resident, Department of Radiodiagnosis, Govt. Medical College and Rajindra Hospital, Patiala, Punjab, India.
3 Dimple Mittal, Amravati Enclave, Near Choukhi Dhani, Panchkula, Haryana, India.
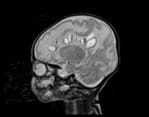
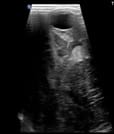
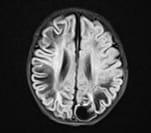
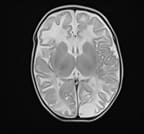
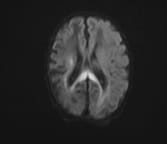
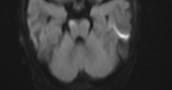
Background: Hypoxic ischemic encephalopathy is a serious concern among asphyxiated newborns due to the associated long term sequelae like cognitive impairment and cerebral palsy. Though the incidence of hypoxic injury remains higher in preterm babies due to incomplete brain maturation, it can occur in term babies as well despite institutional deliveries due to an array of unavoidable fetal, maternal and placental causes. Aims: This study was conducted as an attempt to evaluate the risk factors, to study the correlation between the term of pregnancy with TCUS and MRI imaging findings in HIE and characterise patterns of CNS involvement. Materials and methods: It was a cross-sectional study carried on 50 neonates with clinically diagnosed HIE presenting to the Department of Radiodiagnosis, Rajindra Hospital Patiala who were subjected to transcranial sonography and MRI. Results and Conclusion: This study demonstrated term infants have significant involvement of basal ganglia thalamus type (central) pattern of involvement and preterm infants have periventricular leukomalacia type (white matter injury) of a pattern of involvement. The overall sensitivity and specificity of TCUS in detecting imaging findings in children with clinically diagnosed HIE compared to MRI was found to be 70.45% and 50% respectively, yielding the overall diagnostic accuracy of TCUS as 68% compared to MRI. TCUS can depict central and white matter abnormalities better than peripheral lesions. However MRI provides additional diagnostic information in many cases and can detect precisely the extent of brain injury.
Keywords: Hypoxic Ischemic Encephalopathy, Periventricular Leukomalacia, Transcranial Ultrasound, Magnetic Resonance Imaging, Germinal Matrix Hemorrhage
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Junior Resident, Department of Radiodiagnosis, Govt. Medical College and Rajindra Hospital, Patiala, Punjab, India. Email: |
Mathur M, Gupta I, Mittal D. Evaluation of spectrum of MRI findings in children with Hypoxic Ischemic Encephalopathy and its comparison with transcranial sonography. Int J Med Res Rev. 2021;9(2):87-96. Available From https://ijmrr.medresearch.in/index.php/ijmrr/article/view/1274 |


 ©
©