Study of functional outcome in low grade spondylolisthesis operated by pedicular screw instrumentation and fusion
C. Panchal L.1, L Sarukte V.2*, N Bhanushali R.3
DOI: https://doi.org/10.17511/ijmrr.2021.i01.05
1 Lalit C. Panchal, Honorary Professor, K.B. Bhaba Hospital, Mumbai, Maharashtra, India.
2* Vijay L Sarukte, Additional Associate Professor, K.B. Bhaba Hospital, Mumbai, Maharashtra, India.
3 Ravi N Bhanushali, (DNB), Spine Specialist, K.B. Bhaba Hospital, Mumbai, Maharashtra, India.
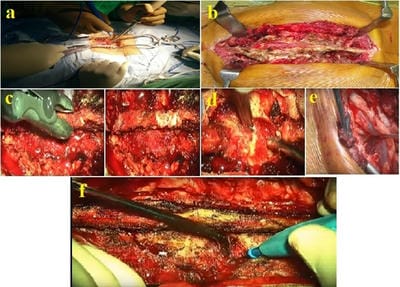
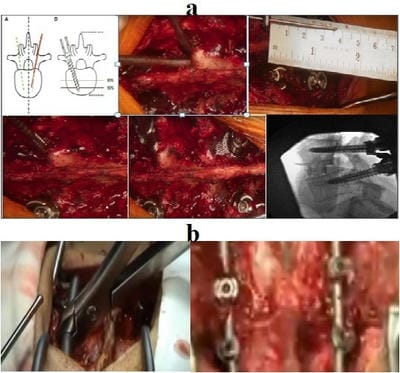
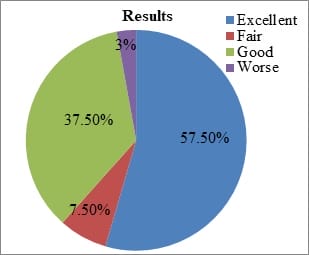
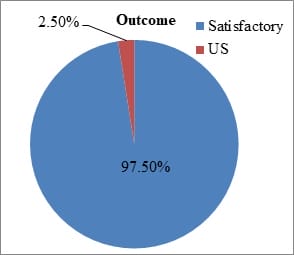
Background: Functional outcome following instrumental spinal surgery for spondylolisthesis in physically energetic patients is crucial. The present study was undertaken to evaluate the functional outcome of low-grade spondylolisthesis accompanied by low back pain with or without radiculopathy, with standard surgical procedure posterior lumbar interbody fusion with instrumentation. Method: In this study total of 40 patients were operated on for low-grade spondylolisthesis by posterior stabilization using a pedicular screw rod system and posterior lumbar interbody fusion. All the patients were followed up till 6 months after surgery and functional outcomes were noted. Results: Assessment of this series it was observed that, 57.5% of the patient had excellent outcome, 37.5% had a good outcome and 97.5% of the study population had satisfactory outcome (improvement in clinical results). There was a significant improvement in pain intensity, walking, lifting, standing, sleeping after surgery. The mean ODI difference between preoperative and post-operative at 6 months follow up was 36.12% (16.75). In the outcome, 62.5% of the patient consisted of severe disability and 32.5% were with moderate disability (total-95%) while postoperative 87.5% were with a minimal disability and only 2.5% of the study population had worsened i.e crippled. Conclusion: The study concluded that surgery in form of decompression with instrumentation and posterior lumbar interbody is a safe and effective method to treat spondylolisthesis.
Keywords: Spondylolisthesis, Radiculopathy, Posterior, Pedicular screw, Fusion, Functional outcome
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Additional Associate Professor, K.B. Bhaba Hospital, Mumbai, Maharashtra, India. Email: |
Panchal LC, Sarukte VL, Bhanushali RN. Study of functional outcome in low grade spondylolisthesis operated by pedicular screw instrumentation and fusion. Int J Med Res Rev. 2021;9(1):34-40. Available From https://ijmrr.medresearch.in/index.php/ijmrr/article/view/1258 |


 ©
©