Study of ANC and immediate PNC mothers admitted with severe anemia in GMC Chandrapur
V Shrirame D.1*, Waikar M.2
DOI: https://doi.org/10.17511/ijmrr.2021.i01.06
1* Deepti V Shrirame, Assistant Professor, Department of Obstetrics and Gynecology, Chandrapur, Maharashtra, India.
2 M.R. Waikar, Professor and HOD, Department of Obstetrics and Gynecology, Chandrapur, Maharashtra, India.
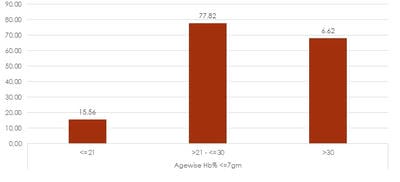
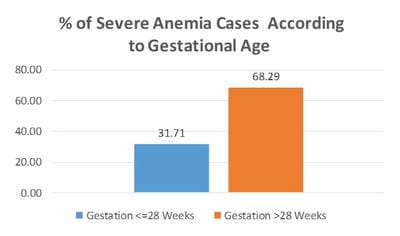
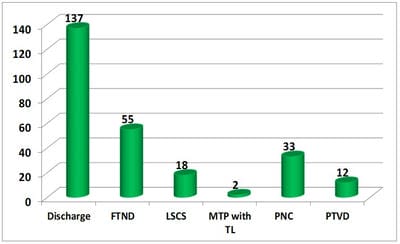
Maternal mortality continues to be a major health problem in the developing world. About 20% of cases of maternal mortality are due to anemia (preventable cause). Objectives: 1. To define the geographical areas around Chandrapur from where the cases of anemia are referred. 2. To co-relate variables like maternal age, gestational age, parity and the time elapsed between last childbirth and current pregnancy. Materials and Methods: Hb of ANC and immediate PNC patients referred with severe anemia was estimated with Sahli’s Haemoglobinometer. Inclusion criteria: 257 ANC and immediate postpartum patients admitted between July 2016 to September 2016 with severe anemia and transfused with blood. Exclusion criteria: anemia due to acute blood loss.Results: 77.8% severe anemia cases were between 21 to 30 years.22% were from Chandrapur taluka.12.8%cases from Rajura and10.12% from Korpana taluka,68.26% cases had gestational age more than 28 weeks.59.92%cases were multipara. In 84.42% of cases last childbirth was less than 3 years.20%cases were of sickle cell anemia patients. There were no cases of abruption placentae, surgical wound infection and maternal mortality. No patient had postpartum haemorrhage as were managed with active management of the third stage of labour and prophylactic 3 tablets of misoprostol per rectum. There were 12 preterm deliveries with no intrauterine deaths. Conclusion: Peripheral preventive services must be strengthened on a priority basis in Chandrapur, Ballarpur, Rajura and Korpana talukas which belong to south Chandrapur where the tribal area is predominant. Probable causes in these areas might be related to culture, ignorance, dietary habits and availability of medical staff which needs to be addressed. Effective counselling regarding early registration, restriction of parity, contraception for spacing births, diet and iron and folic acid supplementation is essential for preventing anemia.
Keywords: Severe anemia, Maternal mortality, ANC, PNC
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Assistant Professor, Department of Obstetrics and Gynecology, Chandrapur, Maharashtra, India. Email: |
Shrirame DV, Waikar MR. Study of ANC and immediate PNC mothers admitted with severe anemia in GMC Chandrapur. Int J Med Res Rev. 2021;9(1):41-45. Available From https://ijmrr.medresearch.in/index.php/ijmrr/article/view/1242 |


 ©
©