Study of knowledge, perception, and practice of patients regarding fasting requirements for blood glucose testing
Hazra A.1*, Mandal S.2, L. Jawalekar S.3, Rawtani J.4, Marlecha M.5
DOI: https://doi.org/10.17511/ijmrr.2021.i01.01
1* Asmita Hazra, Assistant Professor, Department of Biochemistry, Government Medical College, Pali, Rajasthan, India.
2 Saptarshi Mandal, Associate Professor, Department of Transfusion Medicine and Blood Bank, All India Institute of Medical Sciences (AIIMS), Jodhpur, Rajasthan, India.
3 Seema L. Jawalekar, Professor and Head, Department of Biochemistry, Government Medical College, Pali, Rajasthan, India.
4 Jairam Rawtani, Senior Professor and Head, Department of Biochemistry, Dr. Sampurnanand Medical College, Jodhpur, Rajasthan, India.
5 Minal Marlecha, MBBS Student, Government Medical College, Pali, Rajasthan, India.
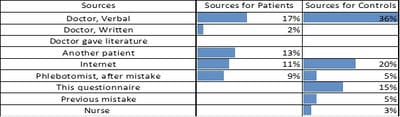
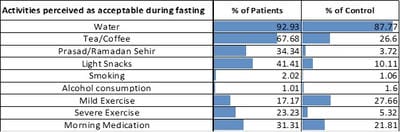
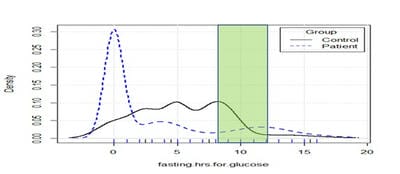
Background: Patient preparation is one of the least standardized parts of the preanalytic phase of testing. Fasting blood glucose requires fasting for 8-12 hours as per various guidelines and also has several other requirements. Lack of communication, understanding, or compliance regarding hours-of-fasting, water-intake, avoidance of caloric snack/beverage, the sudden change in smoking, exercise, alcohol, medication, etc. introduces preanalytic errors. Method: To evaluate awareness, understanding, and compliance with fasting requirements, a face-to-face survey was done on outpatients in a Government Hospital in Pali, Rajasthan, India. Relatively more educated internet users were surveyed as controls through an online SurveyMonkey tool. Results: 98 patients and 187 controls participated in the study. Perception about fasting requirements ranged from 0-17 hours. 71% of patients and 35% of controls perceived that nobody explained to them the duration or nature of fasting. The different sources of information had been used in different proportions by patients and controls. For imparting understanding and compliance about duration, and other requirements of fasting, the instruction was usually incomplete but still much more effective (p-value=0.000002) than formal education level (p-value=0.024). Conclusion: 71% of patients and 35% of controls did not receive instructions for fasting. 40% of those instructed showed better compliance, but awareness was incomplete. The instruction was more effective than formal education in improving awareness and compliance. Improved awareness was strongly associated with receiving instruction and weakly associated with formal education but financial status showed only a weak negative association.
Keywords: Fasting for Diagnostic Laboratory Tests, Patient Preparation, Under-fasting and Over-fasting
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Assistant Professor, Department of Biochemistry, Government Medical College, Pali, Rajasthan, India. Email: |
Hazra A, Mandal S, Jawalekar SL, Rawtani J, Marlecha M. Study of knowledge, perception, and practice of patients regarding fasting requirements for blood glucose testing. Int J Med Res Rev. 2021;9(1):01-12. Available From
https://ijmrr. medresearch.in/index.php/ijmrr/article/view/1240 |


 ©
©