Role of high-frequency USG in rotator cuff injury and its comparison with MRI
Maravi P.1*, Khadiya A.2, Kaushal L.3, Goyal S.4, Patil P.5
DOI: https://doi.org/10.17511/ijmrr.2020.i06.12
1* Poornima Maravi, Associate Professor, Department of Radiodiagnosis, Gandhi Medical College and Hamidia Hospital, Bhopal, Madhya Pradesh, India.
2 Ajay Khadiya, Junior Resident III, Gandhi Medical College and Hamidia Hospital, Bhopal, Madhya Prdaesh, India.
3 Lovely Kaushal, Professor and HOD, Department of Radiodiagnosis, Gandhi Medical College and Hamidia Hospital, Bhopal, Madhya Pradesh, India.
4 Swati Goyal, Associate Professor, Department of Radiodiagnosis, Gandhi Medical College and Hamidia Hospital, Bhopal, Madhya Pradesh, India.
5 Pinki Patil, Assistant Professor, Department of Radiodiagnosis, Gandhi Medical College and Hamidia Hospital, Bhopal, Madhya Pradesh, India.
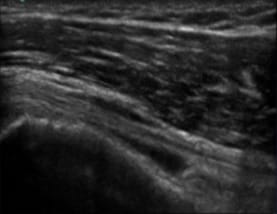
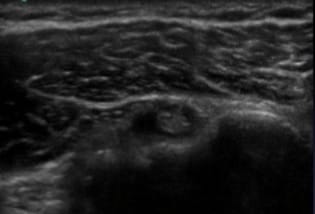
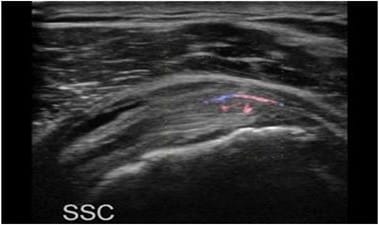
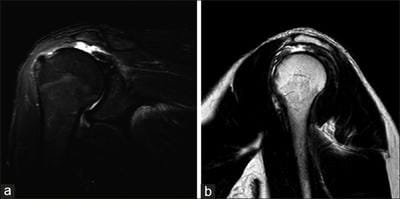
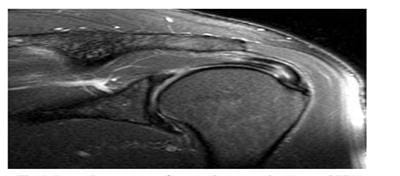
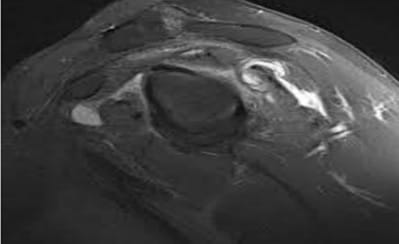
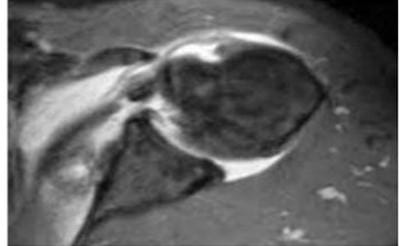
Introduction: Rotator cuff injury is one of the common causes of long-term shoulder pain and disability encountered in the orthopedic clinic. The spectrum of rotator cuff injury includes tendonitis, partial tears, and complete tears. They also may influence the development of the degenerative disease of glenohumeral joint and rotator cuff arthropathy. Material and Methods: The present, prospective study entitled “Role of high-frequency USG in rotator cuff injury and its comparison with MRI” was conducted in the Department of Radiodiagnosis on a total of 100 patients who presented with signs and symptoms of shoulder joint injury in Department of Orthopedic who were then referred for USG and MRI examination to the Department of Radiodiagnosis. Result: Mean age of the patients was 38.26±14.51 years and the majority of patients belonged to the 3rd decade (34%). About 7% of patients belonged to the 2nd decade, 18% of patients each belonged to the 4th and 5th decades of age group. Only 8% and 7% of patients in the present study belonged to extremes of age i.e. >60 years and <20 years respectively. Conclusion: Based on the findings of the present study, it is concluded that rotator cuff injuries are commonly encountered conditions in routine practice, and males are commonly affected as compared to females.
Keywords: MRI, USG, Rotator cuff, Cuff injuries
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Associate Professor, Department of Radiodiagnosis, Gandhi Medical College and Hamidia Hospital, Bhopal, Madhya Pradesh, India. Email: |
Maravi P, Khadiya A, Kaushal L, Goyal S, Patil P. Role of high-frequency USG in rotator cuff injury and its comparison with MRI. Int J Med Res Rev. 2020;8(6):440-450. Available From https://ijmrr.medresearch.in/index.php/ijmrr/article/view/1237 |


 ©
©