Effectiveness of underlay myringoplasty in inactive mucosal chronic otitis media; a prospective study
Swapna U.P.1*, Smitha B.2, Kumar K. S.3
DOI: https://doi.org/10.17511/ijmrr.2020.i06.04
1* Swapna U.P., Associate Professor, Department of ENT, SUT Academy of Medical Sciences, Trivandrum, Kerala, India.
2 Smitha B., Assistant Professor, Department of ENT, SUT Academy of Medical Sciences, Trivandrum, Kerala, India.
3 Salil Kumar K., Professor, Department of ENT, SUT Academy of Medical Sciences, Trivandrum, Kerala, India.
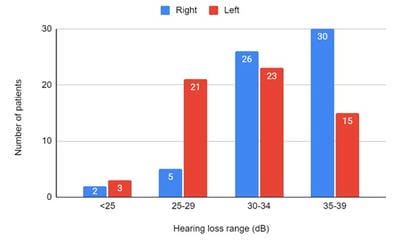
Introduction: Patients with a mucosal type of chronic otitis media (COM) usually have recurrent ear discharge and conductive hearing loss. It is characterized by the central perforation of the tympanic membrane. Myringoplasty is an operation performed to repair tympanic membrane perforation when there is no ossicular damage. It helps to prevent ear discharge and improves hearing. Different techniques used for myringoplasty are underlay and overlay. Underlay technique is an effective procedure for tympanic membrane repair. Methods: 125 patients who underwent underlay myringoplasty over two years in a tertiary care center in Kerala were included in the study. Patients with actively discharging ears were excluded from the study. Results: The majority of the patients were in the age group of 20-29 years (49.6%). There were 47 males (37.6%) and 78 females (62.4%). In 63 patients the surgery was done on the right side (50.4%) and in 62 patients on the left side (49.6%). Maximum preoperative hearing loss was in the range of 30-34 dB (39.2%). 100 patients (80%) showed successful graft uptake with the improvement of hearing in the range of 10-15 dB. Eight patients (6.4%) showed small residual perforation with the improvement of hearing. In 17 patients (13.6%) there was a complete rejection of graft with continuous ear discharge and no improvement in hearing. Conclusion: Underlay myringoplasty is an effective surgical technique for the repair of tympanic membrane perforations in terms of graft take up and improvement of hearing.
Keywords: Tympanic membrane, Chronic otitis media, Myringoplasty, Underlay technique
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Associate Professor, Department of ENT, SUT Academy of Medical Sciences, Trivandrum, Kerala, India. Email: |
Swapna U P, Smitha B, Kumar K S. Effectiveness of underlay myringoplasty in inactive mucosal chronic otitis media; a prospective study. Int J Med Res Rev. 2020;8(6):398-403. Available From https://ijmrr.medresearch.in/index.php/ijmrr/article/view/1229 |


 ©
©