Vaginal progesterone in prevention of preterm labour
Sahoo P.1, Kumar Patel N.2*, Patel O.3, Panigrahi A.4, Biswal S.5, Rath B.6
DOI: https://doi.org/10.17511/ijmrr.2020.i06.13
1 Prativa Sahoo, Junior Resident, Department of Pharmacology, Veer Surendra Sai Institute of Medical Sciences and Research, Burla, Odisha, India.
2* Nayan Kumar Patel, Assistant Professor, Department of Cardiology, Veer Surendra Sai Institute of Medical Sciences and Research, Burla, Odisha, India.
3 Ojaswini Patel, Associate Professor, Department of Obstetrics & Genecology, Veer Surendra Sai Institute of Medical Sciences and Research, Burla, Odisha, India.
4 A.K Panigrahi, Associate Professor, 5 S.B. Biswal, Associate Professor, 6 Bhabagrahi Rath, HOD, 4,5,6 authors are afffiliated with Department of Pharmacology, Veer Surendra Sai Institute of Medical Sciences and Research, Burla, Odisha, India.
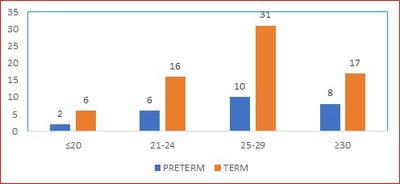
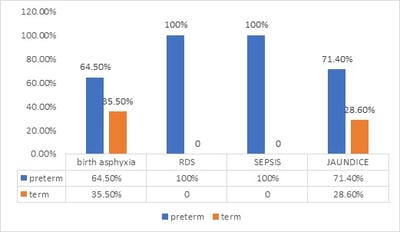
Introduction: Preterm birth, defined as childbirth occurring at less than 37 completed weeks or 259 days of gestation since the first day of a woman’s last menstrual period, is one of the leading causes of neonatal morbidity and mortality. Across 184 countries, the rate of preterm birth ranges from 5% to 18% of babies born. Out of 27 million babies born every year (2018 data ) in India, 3.5 million babies born are premature. Recent literature review has shown that the use of Progesterone reduces risk of preterm birth. But there is little information available regarding the role of Progesterone in preventing preterm labour. Objectives: Primary objective of the study is to find out the incidence of preterm labour among pregnant women taking vaginal progesterone. Secondary objective is toassess the safety and efficacy of progesterone in feto-maternal outcome. Methods: This is a cross sectional study where100 prescriptions from IPD of Dept of O&G, VIMSAR, Burla of women who had recently undergone labour with singleton gestation and with previous history of preterm labour were analysed. Incidence of preterm labour among those taking and not taking vaginal progesterone were compared. Results: There was decreased incidence of preterm labour as there is prolongation mean Gestational age by 9.383 weeks among pregnant women taking vaginal progesterone. Conclusions: In the present study, women taking vaginal progesterone had significantly lowered incidence preterm birth rate.
Keywords: Gestational age, Preterm birth, Singleton gestation, Vaginal progesterone
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Assistant Professor, Department of Cardiology, Veer Surendra Sai Institute of Medical Sciences and Research, Burla, Odisha, India. Email: |
Sahoo P, Patel NK, Patel O, Panigrahi AK, Biswal SB, Rath B. Vaginal progesterone in prevention of preterm labour. Int J Med Res Rev. 2020;8(6):451-456. Available From https://ijmrr.medresearch.in/index.php/ijmrr/article/view/1225 |


 ©
©