Role of pleural biopsy in patients of undiagnosed exudative pleural effusion
Sanwalka N.1, Kumar R.2, Sanwalka M.3*
DOI: https://doi.org/10.17511/ijmrr.2020.i03.08
1 Nidhi Sanwalka, Post graduate resident, Rukmani Devi Beni Prasad Jaipuria Hospital, Jaipur, Rajasthan, India.
2 Ramesh Kumar, Post Graduate Resident, Rukmani Devi Beni Prasad Jaipuria Hospital, Jaipur, Rajasthan, India.
3* Madhvi Sanwalka, Post Graduate Resident, National Institute of Medical Sciences and Research, Jaipur, Rajasthan, India.
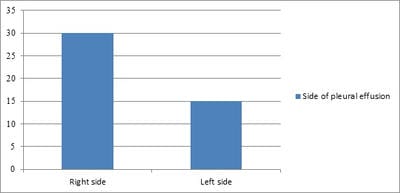
Introduction: Sometimes etiological diagnosis of pleural fluid is not possible by cytology, biochemical and microbiological examinations and labeled as undiagnosed exudative pleural effusion. Our aim of this study to make an etiological diagnosis in such undiagnosed exudative cases with pleural biopsy. Material and method: In this study patients with undiagnosed exudative pleural effusion, where the diagnosis was not made by laboratory investigations were included. Pleural tissue was obtained by Abram’s Needle and sent for histopathology and culture to find mycobacterium tuberculosis. Result: Out of 45 patients 34 (75.5%) were males and 11 (24.5%) were females. The side of pleural effusion was right-sided in 30 (66.6%) and left-sided in 15 (33.4%). The mean value of polymorphs and lymphocytes count was 7.24% and 92.76% respectively. Pleural fluid was hemorrhagic in 10 (22.22%) patients, straw-colored in 30 (71.11%) patients, and clear in 5 (11.11%) patients. The mean level of glucose was 65.66 mg/dl, the lowest being nil and highest being 110 mg/dl. The mean level of protein was 5.54 gm/dl (range 3.7-7.21 gm/dl). The mean value of the pH of pleural fluid was 65.44. Histopathology showed granulomatous inflammation compatible with tuberculosis in 24 (53.3%) cases, metastatic malignancy in 7 (15.5%) cases, chronic inflammation in 10 (22.3%) cases. In 4 (8.9%) cases pleural tissue was inadequate to give any opinion. Among 7 cases of malignancy, 5 (71.42%) cases showed adenocarcinomas and 2 (28.58%) cases showed squamous cell carcinoma. Conclusion: This study suggests that tuberculosis and malignancy are the two common etiologies for exudative pleural effusion. The role of pleural biopsy is pivotal as it helps in making the diagnosis in the majority of cases where other laboratory investigations fail to provide a diagnosis.
Keywords: Etiology, Exudative, Undiagnosed, Pleural effusion, Pleural biopsy, Tuberculosis, Malignancy
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Post Graduate Resident, National Institute of Medical Sciences and Research, Jaipur, Rajasthan, India. Email: |
Sanwalka N, Kumar R, Sanwalka M. Role of pleural biopsy in patients of undiagnosed exudative pleural effusion. Int J Med Res Rev. 2020;8(3):265-268. Available From https://ijmrr.medresearch.in/index.php/ijmrr/article/view/1194 |


 ©
©