Fibrosarcoma of Maxilla: youngest case report
Vanza B.1*, Rawat A.2, Yadav R.3, Patel U.4
DOI: https://doi.org/10.17511/ijmrr.2020.i06.09
1* Bhavuk Vanza, Assistant Professor, Department of Oral & Maxillofacial Surgery, Government Dental College, Indore, Madhya Pradesh, India.
2 Amit Rawat, Associate Professor, Department of Oral & Maxillofacial Surgery, Government Dental College, Indore, Madhya Pradesh, India.
3 Rashi Yadav, Assistant Professor, Department of Oral & Maxillofacial Surgery, Government Dental College, Indore, Madhya Pradesh, India.
4 Umesh Patel, Professor, Department of Pediatrics, RKDF Medical College, Bhopal, Madhya Pradesh, India.
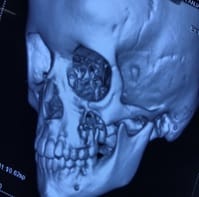
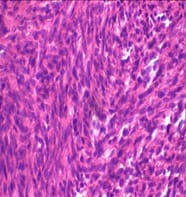
Abstract- Fibrosarcomas are rare but highly fulminant and aggressively malignant neoplasm which occurs as a result of mutated spindle-shaped fibroblasts. According to WHO, they are soft tissue sarcoma commonly present seldom at cutis. The etiology of such a malignancy is obscured nevertheless it has several predisposing factors like pre-existing pathology but the commonest of them is radiation. Mesenchymal malignancies were initially over-diagnosed and were the epicenter of diagnostic dilemma to the pathologist, but with the advent of Vimentin staining and immunohistochemistry, the diagnostic front has fairly advanced for fibrosarcomas. Incidence of Fibrosarcoma in Maxilla accounts for less than 0.1%, when compared to other head and neck malignancies, and is predominantly found between 2nd to 6th decades of life. Various approaches have been documented in the literature regarding its treatment, but aggressive surgical excision remains the mainstay of treating Fibrosarcomas. The role of adjuvant medicinal therapies have been well debated but do have a conclusive outcome. Through this article, we want to highlight and document a case, which occurred at an exceptionally young age, at a site that had no predisposing factors but has proven immunohistochemical diagnosis and was rapidly fulminating and aggressively malignant. The preoperative diagnosis of the patient was inconclusive reporting it to be a mesenchymal tumor, therefore, the patient was treated with the intraoral approach for wide surgical resection. The surgical specimen was subjected to immunohistochemistry with Vimentin staining which reported it to be a Fibrosarcomas, therefore the patient was advised chemotherapy, yet the prognosis is guarded.
Keywords: Fibrosarcoma, Maxilla
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Assistant Professor, Department of Oral & Maxillofacial Surgery, Government Dental College, Indore, Madhya Pradesh, India. Email: |
Vanza B, Rawat A, Yadav R, Patel U. Case Report: Fibrosarcoma in Maxilla in Youngest. Int J Med Res Rev. 2020;8(6):457-460. Available From https://ijmrr.medresearch.in/index.php/ijmrr/article/view/1180 |


 ©
©