Clinical profile and outcome of organophosphorus poisoning in a tertiary care centre, a prospective observational study
Gagarin P.1, Rajagopal R.2*
DOI: https://doi.org/10.17511/ijmrr.2020.i02.02
1 P. Yuri Gagarin, Associate professor, Department of General Medicine, Velammal Medical College Hospital and Research Institute, Madurai, Tamil Nadu, India.
2* R. Lavanya Rajagopal, Associate Professor, Department of Pathology, Velammal Medical College Hospital and Research Institute, Madurai, Tamil Nadu, India.
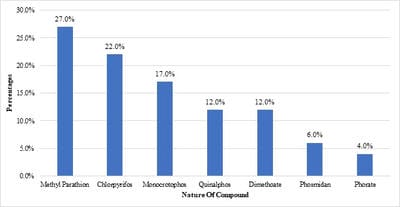
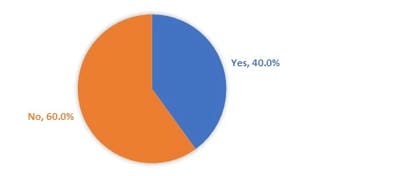
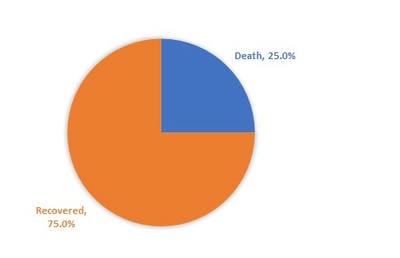
Introduction: Acute organophosphorus (OP) pesticide poisoning is widespread in the developing world. Being predominantly an agricultural country, pesticides and insecticides are used abundantly for cultivation, and access to these poisonous chemical substances by the population is easy. The objectiveof the study was to identifythe nature of the demographic profile, type of compound, clinical manifestations, and outcome of organophosphate poisoning presenting to a tertiary care teaching hospital in India. Material and methods: A cross-sectional study was conducted among 100 patients admitted with OPC poisoning inthe department of general medicine,Velammal Medical College Hospital and Research Institute, Madurai from January 2016 to July 2019. The diagnosis was made based on history or evidence of exposure to OP compound within 24 hours; characteristic manifestations of OP poisoning include, miosis, fasciculations, excessive salivation, improvement of signs and symptoms with administration of atropine were recorded. IBM SPSS version 22 was used for statistical analysis. Results:The majority of the subjects were males(80%). The majority (66%) were in the age group of 21-40 years. The most common OPC to be consumed was Methyl parathion (27%), followed by chlorpyrifos (22%). The major GIT complications were abdominal pain/cramps (100%), followed by nausea and vomiting (83%). Mechanical ventilation was needed in 40% and mortality was reported in 25% of the subjects. Conclusion:OP poisoning affects resonantly males in their economically productive phase of life. Considering the high mortality, adequate strengthening of health services, especially at the primary level is the need of the hour.
Keywords: Organophosphorus, Pesticides, Muscarinic manifestations, Nicotinic manifestations, Poisoning
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Associate Professor, Department of Pathology, Velammal Medical College Hospital and Research Institute, Madurai, Tamil Nadu, India. Email: |
Gagarin PY, Rajagopal RL. Clinical profile and outcome of organophosphorus poisoning in a tertiary care centre, a prospective observational study. Int J Med Res Rev. 2020;8(2):148-153. Available From https://ijmrr.medresearch.in/index.php/ijmrr/article/view/1156 |


 ©
©