Pattern recognition approach and clinico-radiological evaluation of compressive myelopathies at a tertiary care hospital
Kiran J.S.1, Rao M.2, Pasha S.3*
DOI: https://doi.org/10.17511/ijmrr.2020.i01.04
1 Kiran J.S., Postgraduate, Department of Medicine, NRI Medical College and General Hospital, Guntur, Andhra Pradesh, India.
2 M Nageswara Rao, Professor, Department of Neurology, NRI Medical College and General Hospital, Guntur, Andhra Pradesh, India.
3* SK Afsar Pasha, Professor, Department of Neurology, NRI Medical College and General Hospital, Guntur, Andhra Pradesh, India.
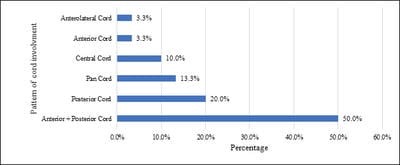
Background: Neuroimaging is indicated in most instances of new-onset myelopathy for clinico-radiological correlation in terms of diagnosis, recovery, and prediction of recurrence. Aim: This study was conducted to study the clinical profile of cases of Compressive Myelopathy and the pattern of spinal cord involvement, also to compare the sites of localisation of clinical diagnosis with MRI diagnosis. Methodology: The present study was a prospective study involving 30 patients. Patients with clinical suspicion of spinal cord disease of age group 20-80 years were included as study participants. The primary pulse sequences included T1 and T2 weighted images on MRI, the location of the lesion, its margins, signal intensity on both T1 and T2 weighted images was noted. Results: The majority of 53.33% of participants were aged between 51 to 60 years. Difficulty in walking was observed in 97% of participants. Men were more often affected than women. Cervical spondylosis was the commonest cause of compressive myelopathy in 57%. A most common pattern of spinal cord involvement was combined Anterior + Posterior cord involvement. The cervical site of localisation (54%) was the commonest followed by the thoracic and lumbar spinal cord. Conclusion: Myelopathies have male preponderance. The commonest cause of compressive myelopathy was Cervical spondylosis. Anterior plus posterior cord syndrome was the commonest pattern seen, followed by posterior cord syndrome, anterior cord syndrome being the least observed. MRI correlates well with a clinical diagnosis and is useful in suggesting the location of the lesion.
Keywords: Cervical spondylosis, Compressive myelopathy, Spinal cord syndromes
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Professor, Department of Neurology, NRI Medical College and General Hospital, Guntur, Andhra Pradesh, India. Email: |
Kiran JS, Rao MN, Pasha SKA. Pattern recognition approach and clinico-radiological evaluation of compressive myelopathies at a tertiary care hospital. Int J Med Res Rev. 2020;8(1):24-30. Available From https://ijmrr.medresearch.in/index.php/ijmrr/article/view/1135 |


 ©
©