Spectrum of MRI abnormalities in pediatric seizures
Mathur M.1, Jeet Singh S.2*, Kaur N.3, Mittal D.4, Garg Y.5, Raikhy A.6
DOI: https://doi.org/10.17511/ijmrr.2020.i01.11
1 Manoj Mathur, Professor, Department of Radiodiagnosis, Govt. Medical College and Rajindra Hospital, Patiala, Punjab, India.
2* Simran Jeet Singh, Junior Resident, Department of Radiodiagnosis, Govt. Medical College and Rajindra Hospital, Patiala, Punjab, India.
3 Navpreet Kaur, Senior Resident, Department of Pediatrics, Post Graduate Institute of Medical Education & Research, Chandigarh, Punjab, India.
4 Dimple Mittal, Junior Resident, Department of Radiodiagnosis, Govt. Medical College and Rajindra Hospital, Patiala, Punjab, India.
5 Yogesh Garg, Junior Resident, Department of Radiodiagnosis, Govt. Medical College and Rajindra Hospital, Patiala, Punjab, India.
6 Ankit Raikhy, Consultant Minimal Access Surgery, Department of Radiodiagnosis, Govt. Medical College and Rajindra Hospital, Patiala, Punjab, India.
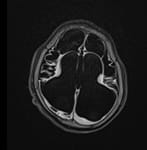
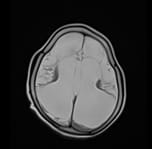
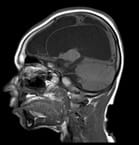
Background: Seizure is a pediatric emergency. Accurate determination of the etiology of seizures is very important to start an effective treatment. The study aims to determine the spectrum of Imaging abnormalities by Magnetic Imaging Resonance (MRI) in children who presented with seizures. Methods: It is a hospital-based prospective observational study which was carried out in Government Medical College and Rajindra Hospital, Patiala. This study included 50 pediatric patients in the age group between 0 months to 18 years who were referred to the Department of Radiodiagnosis for brain MRI between October 2017 to September 2019. Results: Neuroimaging abnormality was found in 19 (38%) cases. 31 (62%) patients had no abnormal finding. The most common imaging findings were inflammatory granuloma in 5 (10%) patients. Other findings were- Hypoxic-ischemic injury (HII) in 4 (8%), Mesial temporal sclerosis in 2(4%), cerebral atrophy in 1(2%), Hemorrhage in 1(2%), Tuberous sclerosis in 1(2%), Focal cortical dysplasia in 1(2%), Lissencephaly in 1 (2%), Joubert syndrome in 1(2%), and Arachnoid cyst in 1 (2%) patients. Conclusion: The MRI was able to identify brain lesions in 38% of pediatric patients who presented with seizures. The study revealed inflammatory granuloma as the commonest cause of seizures in children, followed by Hypoxic-Ischemic Injury. Early recognition of potentially treatable diseases helps in timely treatment and arrest of disease progression. It is recommended to use MRI as a primary investigation during the evaluation and management of pediatric seizures.
Keywords: Hypoxic ischemic injury, Inflammatory granuloma, Neurocysticercosis, Seizures
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Junior Resident, Department of Radiodiagnosis, Govt. Medical College and Rajindra Hospital, Patiala, Punjab, India. Email: |
Mathur M, Singh SJ, Kaur N, Mittal D, Garg Y, Raikhy A. Spectrum of MRI abnormalities in pediatric seizures. Int J Med Res Rev. 2020;8(1):69-75. Available From https://ijmrr.medresearch.in/index.php/ijmrr/article/view/1120 |


 ©
©