Dosimetric comparison and clinical correlation between conventional four field radiotherapy versus three-dimensional conformal radiotherapy in cancer cervix
Agarwal S.1, Kumar Chauhan A.2*, Kumar P.3, Nigam J.4, Kumar P.5
DOI: https://doi.org/10.17511/ijmrr.2019.i06.13
1 Shubhi Agarwal, Senior Resident, Department of Radiation Oncology, Shri Ram Murti Smarak Institute of Medical Sciences, Bareilly, Uttar Pradesh, India.
2* Arvind Kumar Chauhan, Associate Professor, Department of Radiation Oncology, Shri Ram Murti Smarak Institute of Medical Sciences, Bareilly, Uttar Pradesh, India.
3 Piyush Kumar, Professor, Department of Radiation Oncology, Shri Ram Murti Smarak Institute of Medical Sciences, Bareilly, Uttar Pradesh, India.
4 Jitendra Nigam, Assistant Professor cum RSO, Department of Radiation Oncology, Shri Ram Murti Smarak Institute of Medical Sciences, Bareilly, Uttar Pradesh, India.
5 Pavan Kumar, , Department of Radiation Oncology, Shri Ram Murti Smarak Institute of Medical Sciences, Bareilly, Uttar Pradesh, India.
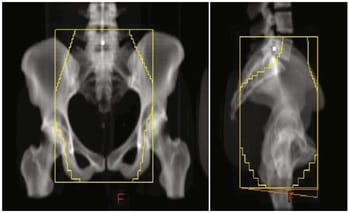
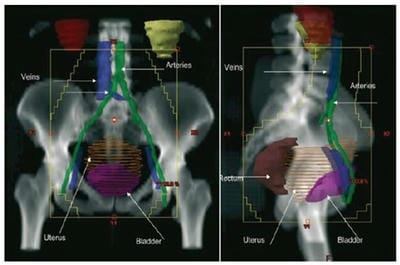
Introduction: With sectional imaging, wide variations are reported in pelvic anatomy of individual patients raising concerns over adequate coverage of target volume with conventional radiotherapy based on standard bony landmarks. Three-dimensional conformal radiotherapy (3DCRT) is reported to decrease normal tissue toxicity, along with decrease in chances of geographic miss. Materials and Methods: Fifty patients of cancer cervix underwent planning contrast enhanced CT scan. Target volumes & OAR were contoured. Patients were randomized into conventional & conformal arms. Conventional fields were planned using standard bony landmarks. Results: Field sizes used for the 3DCRT plans were significantly larger than those used for the conventional plans (p= 0.000). Optimal PTV coverage was significantly improved using 3DCRT as compared to conventional radiotherapy (p= 0.0001). Dose homogeneity in both arms were almost similar (p= 0.292), while conformity index was better in 3DCRT which was statistically significant between the groups (p= 0.000). Conclusion: The present study showed significantly better target volume coverage & dose homogeneity with 3DCRT which may translate into better local control & survival but longer follow up is required to validate it.
Keywords: Cancer cervix, Conventional radiotherapy, Three-dimensional conformal radiotherapy
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Associate Professor, Department of Radiation Oncology, Shri Ram Murti Smarak Institute of Medical Sciences, Bareilly, Uttar Pradesh, India. Email: |
Agarwal S, Chauhan AK, Kumar P, Nigam J, Kumar P. Dosimetric comparison and clinical correlation between conventional four field radiotherapy versus three-dimensional conformal radiotherapy in cancer cervix. Int J Med Res Rev. 2019;7(6):526-535. Available From https://ijmrr.medresearch.in/index. php/ijmrr/article/view/1112 |


 ©
©