A study to assess the quality of life (QOL) of patients suffering from tinea corporis attending dermatology OPD of a tertiary care centre of Eastern India
Kumar Das N.1, Das S.2*
DOI: https://doi.org/10.17511/ijmrr.2019.i06.08
1 Nirmalya Kumar Das, Tutor, Department of Dermatology, Venereology and Leprosy, NRS Medical College, Kolkata, West Bengal, India.
2* Suchibrata Das, Assistant Professor, Department of Dermatology, Venereology and Leprosy, NRS Medical College, Kolkata, West Bengal, India.
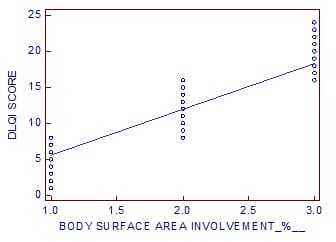
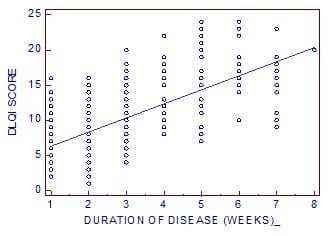
Background: A huge number of patients in our country are affected by Tinea Corporis (TC). The number of patients affected by dermatophytosis has increased by a large extent in the last 4 to 5 years. The quality of life in TC patients can be affected by various factors including the disease morbidity, duration of disease, social & demographic factors. Aims and Objectives: The aim of the study is to find out the effect of TC on the quality of life of the affected patients & along with that to assess whether there is some association of this effect on quality of life with some demographic & clinical factors. Methods: The effect on quality of life of 328 patients affected by TC who attended the Dermatology outpatient’s department of NRS Medical College was assessed using the Dermatology Life Quality Index (DLQI) questionnaire. Results: 12 (3.658%) of the patients had an extremely large effect on quality of life. There was a very large effect on the QOL of 121 (36.890%) patients. There was moderate effect on 134 (40.853 %) of the patients. There was a small effect on 59 (17.987 %) of the patients. 2 (0.609 %) patients had no effect on their QOL. Duration of disease & body surface area involved have significant impacts on QOL. Conclusion: The quality of life is adversely affected by TC. Early detection & treatment of the disease is very important. Steps must be taken to increase awareness about the disease among the general population.
Keywords: Tinea Corporis, Quality of life, Dermatology Life Quality Index (DLQI)
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Assistant Professor, Department of Dermatology, Venereology and Leprosy, NRS Medical College, Kolkata, West Bengal, India. Email: |
Das NK, Das S. A study to assess the quality of life (QOL) of patients suffering from tinea corporis attending dermatology OPD of a tertiary care centre of Eastern India. Int J Med Res Rev. 2019;7(6):496-503. Available From https://ijmrr.medresearch.in/index.php/ijmrr/article/view/1103 |


 ©
©