Dosimetric parameters of heart and left ventricle – comparison of 3D CRT and IMRT in left cancer breast
Mehta A.1, Kumar P.2*, Silambarasan N.3, Navitha S.4, Nigam J.5, Kumar P.6, Chauhan A.7
DOI: https://doi.org/10.17511/ijmrr.2019.i06.05
1 Ankita Mehta, Junior Resident, 2* Piyush Kumar, Professor and Head, 3 N.S. Silambarasan, Assistant Professor cum Medical Physicist, 4 S. Navitha, Assistant Professor cum Medical Physicist, 5 Jitendra Nigam, Assistant Professor cum Medical Physicist, 6 Pavan Kumar, Assistant Professor, 7 Arvind Chauhan, Associate Professor; 1,2,3,4,5,6,7author are affiliated with Department of Radiation Oncology, Shri Ram Murti Institute of Medical Sciences, Bareilly, Uttar Pradesh, India.
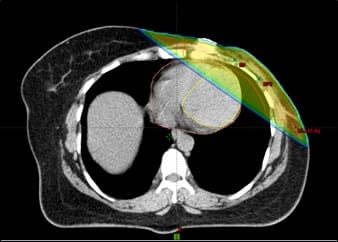
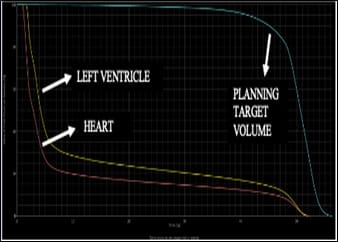
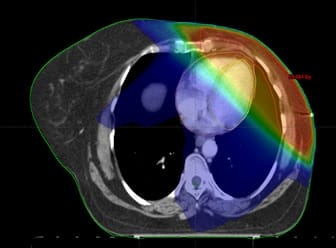
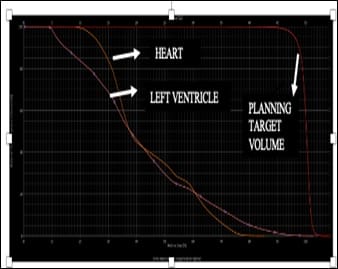
Background: Conformal Radiotherapy techniques adapting to the ballistics of delineated volumes allowed significant reduction in excess radiation induced mortality however the increasing number of long-term survivors and expanding use of cardiotoxic drug highlight the persistent need for maximal cardiac possible sparing. The low dose volume of left ventricle are better predictor of acute coronary events than mean heart dose. Materials and Methods: 38 post-MRM patients were randomized to treatment by 3Dimensional Conformal Radiotherapy (3D CRT) and Intensity Modulated Radiotherapy (IMRT) technique. Two tangential beams were used in 3D CRT technique while five to seven (mostly tangential beams) were used in inversely planned IMRT technique. The dose volume parameters of planning target volume, heart and left ventricle were compared. Results: The dosimetry of Planning target volume showed significantly better coverage in IMRT technique (D90, D95) however the D50 was comparable in both the techniques. In dosimetry of heart, the high dose volumes (V30, V40) were nearly comparable in both the techniques. The other dose volume parameters (V5, V10, V20, V25, D33, D67, D100) and the mean dose were significantly lesser in 3D CRT technique along with significantly better sparing of left ventricle (Dmean and V5). Conclusion: The dosimetry of target volume was better with IMRT technique, but this was accompanied by a huge increase in dose to whole heart and specifically the left ventricle which has strong potential to translate into an increased cardiotoxicity. A better distribution of the target region may be obtained by multiple segmentation of the two tangential fields in 3D CRT plans with further reduction in dose to heart and left ventricle.
Keywords: 3-Dimensional Conformal Radiotherapy (3D CRT), Intensity Modulated Radiotherapy (IMRT), Cardiotoxicity, Planning target volume, Heart, Left ventricle
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Professor and Head, Department of Radiation Oncology, Shri Ram Murti Institute of Medical Sciences, Bareilly, Uttar Pradesh, India. Email: |
Mehta A, Kumar P, Silambarasan NS, Navitha S, Nigam J, Kumar P, Chauhan A. Dosimetric parameters of heart and left ventricle – comparison of 3D CRT and IMRT in left cancer breast. Int J Med Res Rev. 2019;7(6):468-474. Available From https://ijmrr.medresearch.in/index.php/ijmrr/article/view/1096 |


 ©
©