Psoriatic Arthritis in the Eastern Part of Uttar Pradesh
Kumar Bhaskar K.1, Kumar Rai R.2, Mishra A.3, Chawla K.4, Kumar Shukla R.5*
DOI: https://doi.org/10.17511/ijmrr.2021.i05.06
1 Kamlesh Kumar Bhaskar, Consultant, Department of Skin & V.D., District Hospital Gazipur, Gazipur, Uttar Pradesh, India.
2 Rajesh Kumar Rai, Associate Professor, Department of Forensic Medicine, Moti Lal Nehru Medical College, Prayagraj, Uttar Pradesh, India.
3 Archana Mishra, Assistant Professor, Department of Biochemistry, Moti Lal Nehru Medical College, Prayagraj, Uttar Pradesh, India.
4 Kavita Chawla, Professor, Department of Physiology, Moti Lal Nehru Medical College, Prayagraj, Uttar Pradesh, India.
5* Rakesh Kumar Shukla, Assistant Professor, Department of Anatomy, Autonomous State Medical College and Hospital, Mirzapur, Uttar Pradesh, India.
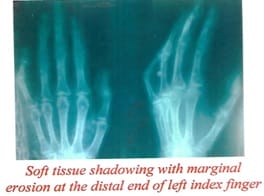
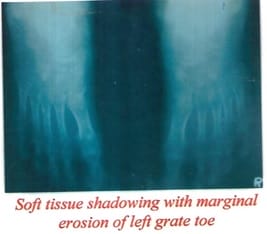
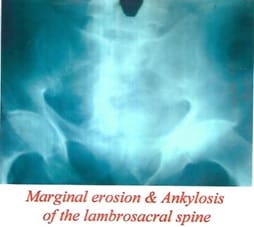
Aim: This original research article aims to study Psoriatic Arthritis in the Eastern Part of Uttar Pradesh. Material & Method: Two hundred twenty-eight patients of psoriasis regardless of age, sex, religion, occupation, attending the skin, and V. D. outpatients Department, B.R.D. Medical College, Gorakhpur for were taken because of the subject of this study. The bulk of patients belonged to the Eastern U.P. and adjoining areas of Bihar and Nepal. The clinical criteria for diagnosis of psoriasis were the presence of Erythematous and papulosquamous lesions with loosely adherent silvery-white scales. The auspitz's sign was demonstrated all told the cases. The detailed clinical history and examination were recorded with Tests for Rheumatoid factor and serum uric acid, Radiographs of both hands and feet, Radiographs of the lumbosacral Spine and both sacroiliac joints and Radiographs of affected joints (if any). Each patient was categorised into mild to severe psoriasis. Result: The total number of psoriatic arthritis cases was found, 26 of which male were 17 and female were 9. The maximum number of Arthritis cases, 18.5%, were seen with severe disease (PASI score > 15) with higher occurrence in males. The maximum number of joints involved distal interphalangeal joint was 69.2 3%, and the minimum number of joints involved was significant joint 7.69%. Conclusion: Psoriasis care is unbalanced, with men being more likely to undergo specialist treatment than women, causing higher distal interphalangeal (D.I.P.) joint arthropathy.
Keywords: Psoriasis, Psoriatic Arthritis, PASI score, PsA Radiology
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Assistant Professor, Department of Anatomy, Autonomous State Medical College and Hospital, Mirzapur, Uttar Pradesh, India. Email: |
Kamlesh Kumar Bhaskar, Rajesh Kumar Rai, Archana Mishra, Kavita Chawla, Rakesh Kumar Shukla, Psoriatic Arthritis in the Eastern Part of Uttar Pradesh. Int J Med Res Rev. 2021;5(9):315-321. Available From https://ijmrr.medresearch.in/index.php/ijmrr/article/view/1324 |


 ©
©