Managing COVID in Homecare – Approach to Treatment, Monitoring, and Follow-up by the Family Physician.
Narayanan V.1*
DOI: https://doi.org/10.17511/ijmrr.2021.i05.03
1* Varsha Narayanan, Consultant, Family Medicine and Holistic Health, Mumbai, Maharastra, India.
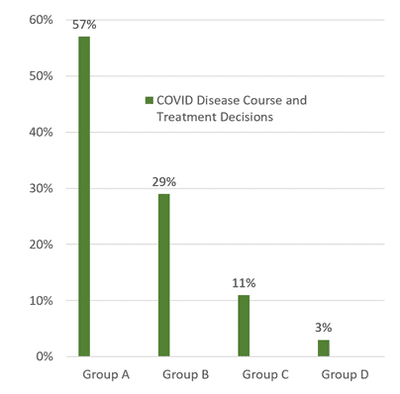
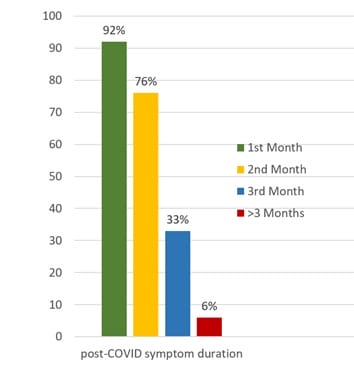
Introduction: The 2nd wave of COVID caused an unprecedented burden on health care workers and resources, calling for structured and effective management of most COVID patients in-home care by general and family physicians via digital and virtual monitoring. Methodology: A systematic treatment approach evolved from COVID diagnosis, homecare determination and isolation, oxygen saturation and temperature monitoring documentation, guidance on proning and breathing techniques, diet and lifestyle measures, evaluating comorbidities, and prescribing appropriate medicines. Timely decision making and stratification to assess disease course and need for hospitalization based on meticulous monitoring, clinical signs and appropriate tests were followed. A balanced approach avoiding unnecessary medication and tests, and allaying panic resulting from multiple information sources, was the novel challenge for physicians. Post-COVID follow up was done for three months. Results: The recovery rate in homecare with this approach was 97%, with only 11% needing corticosteroids in the second week. The need for hospitalization was in 3%. In the first month, > 90% had post-COVID symptoms, mainly lower energy, fatigue, weakness, reduced smell/taste and reduced work capacity. However, by the 3rd month, this reduced to 33%, with only 6% showing symptoms beyond three months. Management was conservative in the majority. Conclusion: A systematic and rational approach to treating, monitoring and managing COVID patients at home can enable better care and recovery and limit unnecessary hospitalization. Diet and lifestyle measures, documentation of oxygen saturation and temperature monitoring, proning and breathing techniques, and psychological support are of great importance that aid recovery and enable sound clinical evaluation.
Keywords: COVID homecare, Oxygen saturation, Proning, Post-COVID, 2nd Wave
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Consultant, Family Medicine and Holistic Health, Mumbai, Maharastra, India. Email: |
Varsha Narayanan, Managing COVID in Homecare – Approach to Treatment, Monitoring, and Follow-up by the Family Physician.. Int J Med Res Rev. 2021;9(5):289-297. Available From https://ijmrr.medresearch.in/index.php/ijmrr/article/view/1315 |


 ©
©