A rare case of iii cranial nerve palsy - mucormycosis involving the right maxillary and ethmoidal sinus
Gandhi K.1*, Sakthivel V.2
DOI: https://doi.org/10.17511/ijmrr.2021.i03.08
1* K. Praveen Gandhi, Post Graduate, Department of Medicine, Vinayaka Mission’s Medical College and Hospital, Vinayaka Mission’s Research Foundation (Deemed to be University) Karaikal, Puducherry, , India.
2 V. Sakthivel, Professor, Department of Medicine, Vinayaka Mission’s Medical College and Hospital, Vinayaka Mission’s Research Foundation (Deemed to be University) Karaikal, Puducherry, , India.
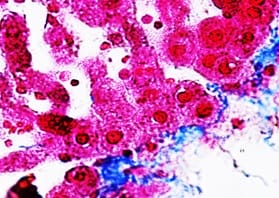
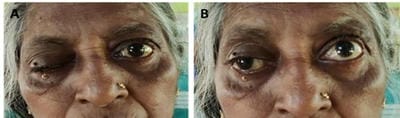
IIIrd Cranial nerve palsy, known as oculomotor nerve palsy, may result from various causes, however, the etiology remains unknown in some instances. This case report aims to present the authors' experience with a case of IIIrd cranial nerve palsy, together with a review of the literature. Many etiologies have been associated with isolated oculomotor nerve palsies. We report the case of a patient who presented with right maxillary and ethmoidal sinusitis with IIIrd cranial nerve palsy associated with mucormycosis. Careful examinations to rule out other causes must be done and then treatment with antifungals should be considered after early diagnosis.
Keywords: Cranial nerve III palsy, Maxillary sinus, Ethmoidal sinus, Mucormycosis
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Post Graduate, Department of Medicine, Vinayaka Mission’s Medical College and Hospital, Vinayaka Mission’s Research Foundation (Deemed to be University) Karaikal, Puducherry, , India. Email: |
Gandhi KP, Sakthivel V. A rare case of iii cranial nerve palsy - mucormycosis involving the right maxillary and ethmoidal sinus. Int J Med Res Rev. 2021;9(3):181-184. Available From https://ijmrr.medresearch.in/index.php/ijmrr/article/view/1285 |


 ©
©