Air-conditioning guidelines for healthcare facilities during the covid pandemic
Sharma A.1, Kumar K R.2, K Patnaik S.3*
DOI: https://doi.org/10.17511/ijmrr.2021.i02.10
1 Ashutosh Sharma, MBBS MD, Professor, Department of Hospital Administration, Armed Forces Medical College, Pune , Maharastra, India.
2 Ramesh Kumar K, MBBS, Resident, Department of Hospital Administration, Armed Forces Medical College, Pune, Maharastra, India.
3* Saroj K Patnaik, MBBS, MHA, Professor, Department of Hospital Administration, Armed Forces Medical College, Pune, Maharashtra, India.
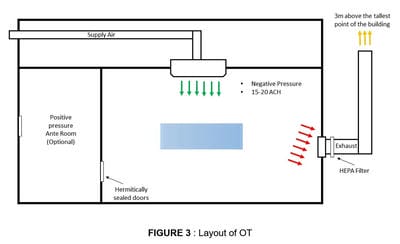
Coronavirus disease (COVID-19) is an infectious disease caused by a newly discovered Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2). The disease spreads primarily through respiratory droplets, physical contact and contact with surfaces as well as fomites. Isolation of patients in hospitals and quarantine of contacts in separate facilities are the mainstay of outbreak containment. This pandemic has brought forward various challenges to the hospital administrators, one of the most important being air-conditioning of hospitals in the time of this pandemic. Paradox to the positive pressure rooms required for critically ill and vulnerable patients, it is negative pressure rooms that are required to contain and avoid the spread of COVID19. This descriptive study provides consolidated guidelines to establish or retrofit the available air-conditioning system at hospitals, at the time of the COVID pandemic.
Keywords: Air-conditioning, COVID-19, Isolation rooms, Negative pressure
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , MBBS, MHA, Professor, Department of Hospital Administration, Armed Forces Medical College, Pune, Maharashtra, India. Email: |
Sharma A, Kumar KR, Patnaik SK. Air-conditioning guidelines for healthcare facilities during the covid pandemic. Int J Med Res Rev. 2021;9(2):109-114. Available From https://ijmrr.medresearch.in/index.php/ijmrr/article/view/1273 |


 ©
©