A descriptive study on the hypertensive crisis in Visakhapatnam, Andhra Pradesh, India
Prakasa Rao S.1*, Sweta Ramani S.2, Sai Kiran P.3, Kiran Prasad S.4
DOI: https://doi.org/10.17511/ijmrr.2020.i06.02
1* Salla Surya Prakasa Rao, Professor, Department of General Medicine, NRI Institute of Medical Sciences, Visakhapatnam, Andhra Pradesh, India.
2 Salla Sweta Ramani, DNB(CTVS), Ex. Registrar, Department of Cardiothoracic Surgery, King George Hospital, Andhra Medical College, Visakhapatnam, Andhra Pradesh, India.
3 Pudi Venkat Sai Kiran, Post-Graduate, Department of General Medicine, NRI Institute of Medical Sciences, Visakhapatnam, Andhra Pradesh, India.
4 Siddanati Kiran Prasad, Internee, Department of General Medicine, NRI Institute of Medical Sciences, Visakhapatnam, Andhra Pradesh, India.
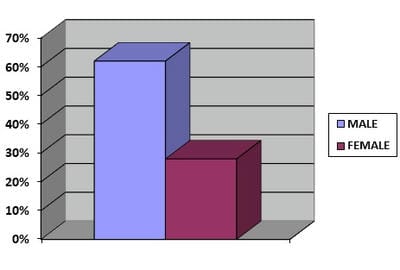
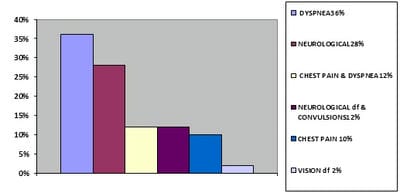
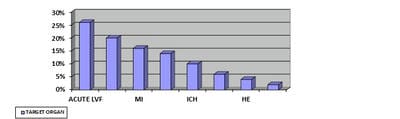
Objective: The objective of the present study, A Descriptive study on Hypertensive Crisis in Visakhapatnam, India was to evaluate the modes of presentations, clinical profile, and spectrum of target organ damage in patients with hypertensive emergencies. Material and Methods: The study population included patients admitted in this hospital with severely elevated blood pressure with clinical or laboratory evidence of acute target organ damage. Result: The clinical and laboratory profile of 50 of these patients were evaluated. Males had higher chances of developing a hypertensive emergency compared to females. The commonest presenting symptoms were chest pain, dyspnoea, and neurological deficit. The majority of the patients have known hypertensives. Higher levels of blood pressure at presentation were associated with an adverse outcome. Acute LVF was the commonest target organ damage observed. In-hospital mortality of 14% was observed in the present study. Conclusion: Known hypertensives are at a higher risk of presenting with acute target organ damage associated with chest pain. Acute LVF is the commonest form of target organ damage encountered in the present study.
Keywords: Hypertensive Crisis, Hypertensive Emergency, Visakhapatnam
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Professor, Department of General Medicine, NRI Institute of Medical Sciences, Visakhapatnam, Andhra Pradesh, India. Email: |
Rao SSP, Ramani SS, Kiran PVS, Prasad SK. A descriptive study on the hypertensive crisis in Visakhapatnam, Andhra Pradesh, India. Int J Med Res Rev. 2020;8(6):386-391. Available From https://ijmrr.medresearch.in/index.php/ijmrr/article/view/1230 |


 ©
©