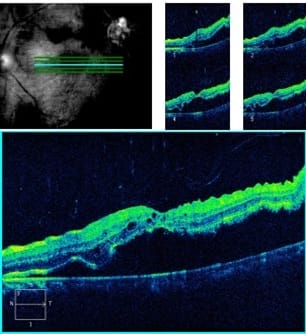
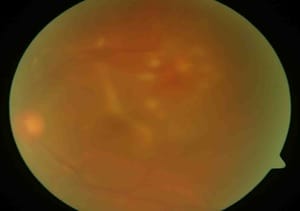
Posterior segment intraocular foreign body with secondary retinal detachment in a phakic eye: a case report
C Porwal A.1*, Jain H.2, Mahajan P.3
DOI: https://doi.org/10.17511/ijmrr.2020.i05.06
1* Amit C Porwal, Senior Consultant Cataract and Head Glaucoma Services, Department of Glaucoma, Choithram Netralaya, Indore, Madhya Pradesh, India.
2 Hardik Jain, Consultant Ophthalmologist, Department of Retina, Choithram Netralaya, Indore, Madhya Pradesh, India.
3 Pratik Mahajan, Consultant Ophthalmologist, Department of Retina, Choithram Netralaya, Indore, Madhya Pradesh, India.
Intraocular foreign bodies (IOFBs) are an important cause of visual loss. The current case describes a case of retained intraocular foreign body with secondary retinal detachment in a phakic eye in a 38-year-old man. The foreign body was safely removed through the sclerotomy port without touching the crystalline lens. The current case report wanted to show the anatomic and visual outcomes of vitreoretinal surgery in such cases.
Keywords: Intraocular foreign body, Retinal detachment, Phakic eye, Visual loss, Visual trauma
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Senior Consultant Cataract and Head Glaucoma Services, Department of Glaucoma, Choithram Netralaya, Indore, Madhya Pradesh, India. Email: |
Porwal AC, Jain H, Mahajan P. Posterior segment intraocular foreign body with secondary retinal detachment in a phakic eye: a case report. Int J Med Res Rev. 2020;8(5):375-378. Available From https://ijmrr.medresearch.in/index.php/ijmrr/article/view/1217 |


 ©
©