Papillary carcinoma of the male breast in a comparatively young patient: A case report of a rare entity
Prashant D.1, Prashant V.2*
DOI: https://doi.org/10.17511/ijmrr.2020.i05.05
1 Dolly Prashant, Associate Professor, Department of Pathology, Government Dental College, Raipur, Chhattisgarh, India.
2* Viplav Prashant, Assistant Professor, Department of Biochemistry, Government Dental College, Raipur, Chhattisgarh, India.
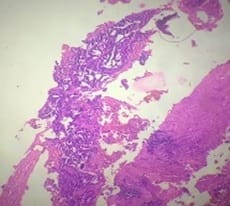
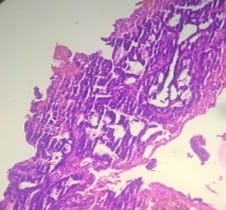
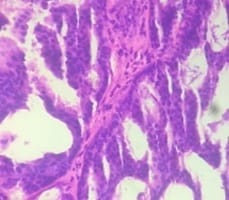
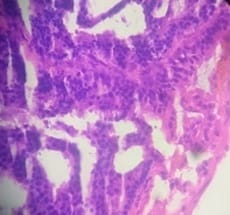
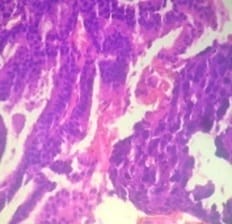
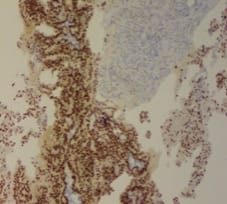
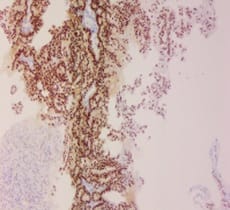
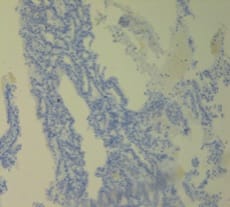
Breast carcinoma in men is rare and intra-cystic papillary carcinoma of male breast is an extremely rare entity. Papillary lesions of male breast comprise of the spectrum of lesions ranging from benign intraductal papilloma to intraductal papillary carcinoma and invasive papillary carcinoma. It occurs most commonly in the seventh decade of life and accounts for <1% of all breast malignancies. The present case report is of a comparatively younger, 37 years old male who presented with a mass on lower quadrant (retro-areolar region) of the left breast.
Keywords: Male breast, Papillary lesions, Intra-cystic papillary carcinoma, Invasive papillary carcinoma
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Assistant Professor, Department of Biochemistry, Government Dental College, Raipur, Chhattisgarh, India. Email: |
Prashant D, Prashant V. Papillary carcinoma of the male breast in a comparatively young patient: A case report of a rare entity. Int J Med Res Rev. 2020;8(5):369-374. Available From https://ijmrr.medresearch.in/index.php/ijmrr/article/view/1214 |


 ©
©