Practical guidance for healthcare professionals during the COVID-19 pandemic; with special emphasis on the care of cardiovascular patients and personal protection
Chugh Y.1, Chugh S.2, Kumar Chugh S.3*
DOI: https://doi.org/10.17511/ijmrr.2020.i03.11
1 Yashasvi Chugh, Chief Fellow, Cardiovascular Medicine, Icahn School of Medicine, Mount Sinai and St. Luke`s Hospital, New York, USA.
2 Sunita Chugh, Consultant, Non–Invasive Cardiology, Jaipur National University Hospital and Medical College, Institute for Medical Sciences and Research Center, Jaipur, Rajasthan, India.
3* Sanjay Kumar Chugh, Head of Department of Cardiology and Interventional Cardiology, Jaipur National University Hospital and Medical College, Institute for Medical Sciences and Research Center, Jaipur, Rajasthan, India.
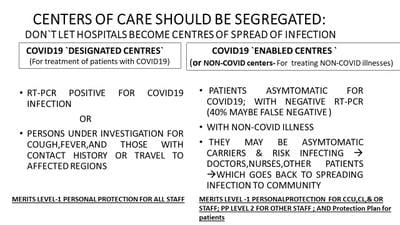
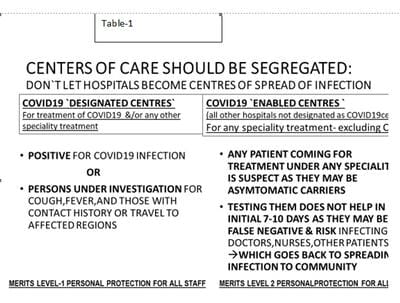
A novel, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is causing the COVID-19 pandemic. There are concerns regarding the spread of disease by asymptomatic carriers to healthcare workers who continue to see patients and to perform procedures on them. The infection then could be transmitted through them to other patients who eventually, could infect persons in the community. Further, limitations of existing tests to detect new cases that are negative early in the disease; and the inability to use appropriate personal protection equipment (PPE)also contribute to the spread of infection. This document, from the COVID-19 Working Group of Wellness and Radial Intervention Society, describes considerations for management and care of cardiovascular disease (CVD) patients with the concept of COVID 19 'designated Vs. enabled' centers for those with symptoms of and/ or confirmed COVID-19 disease Vs. asymptomatic suspects. It also provides guidance to healthcare professionals, hospital administrators, and policymakers in general and to those managing patients with CV and other diseases, regarding the concept of 'levels of personal protection` for staff; with suggestions for 'equivalent innovative alternatives', and 'a protection plan' for patients to prevent the spread of disease.
Keywords: Coronavirus, COVID-19, Cardiovascular disease, Cardiac catheterization laboratory, Echocardiography, Coronary care unit, Invasive, Semi-invasive, and non-invasive procedures, Personal protection equipment (PPE)
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Head of Department of Cardiology and Interventional Cardiology, , Jaipur National University Hospital and Medical College, Institute for Medical Sciences and Research Center, Jaipur, Rajasthan, India. Email: |
Chugh Y, Chugh S, Chugh SK. Practical guidance for healthcare professionals during the COVID-19 pandemic; with special emphasis on the care of cardiovascular patients and personal protection. Int J Med Res Rev. 2020;8(3):277-287. Available From https://ijmrr.medresearch.in/index.php/ijmrr/article/view/1179 |


 ©
©