The necessity of replanning during the intensity-modulated radiotherapy (IMRT) for head and neck cancer, to ensure adequate coverage of target volume
Naveen B.1*, S. Narayanan G.2, Narayanan S.3
DOI: https://doi.org/10.17511/ijmrr.2020.i02.10
1* Naveen B., Assistant Professor, Department of Radiation Oncology, VTSM Peripheral Cancer Centre, Kalaburagi, Karnataka, India.
2 Geeta S. Narayanan, Professor and HOD, Department of Radiation Oncology, Vydehi Institute of Medical Sciences and Research Centre, Bengaluru, Karnataka, India.
3 Sowmya Narayanan, HOD, Department of Radiation Physics, Vydehi Institute of Medical Sciences and Research Centre, Bengaluru, Karnataka, India.
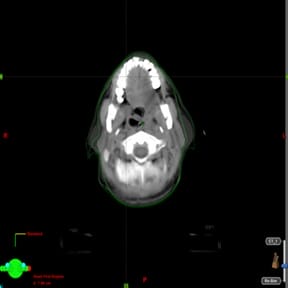
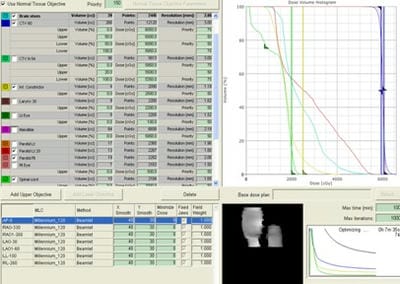
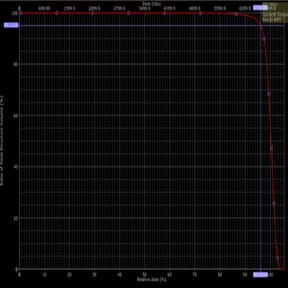
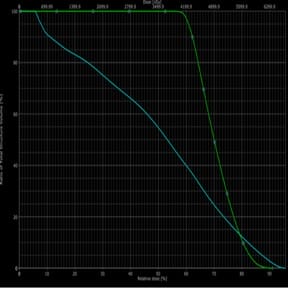
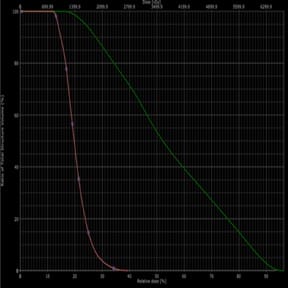
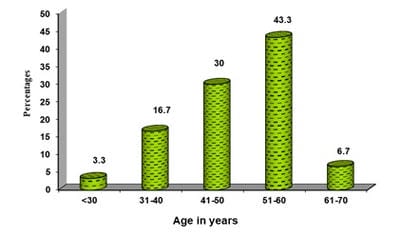
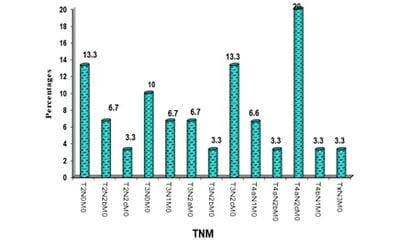
Introduction: In head and neck cancer the location, size, shape of disease, and normal anatomy change in 6-7 weeks radiotherapy. As a result, steep dose gradients move across target and critical structures resulting in underdose to target and overdose to critical structures. Aim: comparison of target coverage in initial IMRT plan and replan and to quantify dose changes to normal structures in two plans. Methods and Material: 30 patients with locally advanced head and neck cancer patients planned for curative radiotherapy were selected and treated with 3DCRT plan. For dosimetric comparison IMRT plan was created for pre-treatment and repeat CT, which was done after 40Gy. Statistical analysis used: Statistical methods (student’s paired t-test) were applied. Results: Both PTV coverage (V95 from 96.29±1.12 to 97.33±0.80) and dose (D95 from 66.64±0.87 to 67.57±0.74) increased in replanned CT. Both max and mean doses to the brainstem and spinal cord along with mean dose to parotid glands increased in replanned CT. Conclusions: Replanning is necessary during mid-treatment to accommodate anatomical and dosimetric changes during curative radiotherapy.
Keywords: Head and Neck cancer, IMRT, Replanning
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Assistant Professor, Department of Radiation Oncology, VTSM Peripheral Cancer Centre, Kalaburagi, Karnataka, India. Email: |
Naveen B, Narayanan GS, Narayanan S. The necessity of replanning during the intensity-modulated radiotherapy (IMRT) for head and neck cancer, to ensure adequate coverage of target volume. Int J Med Res Rev. 2020;8(2):189-200. Available From https://ijmrr.medresearch.in/index.php/ijmrr/article/view/1178 |


 ©
©