Comparison of medical therapy with renal denervation in patients with resistant hypertension
Palaparti R.1*, Syed I.2
DOI: https://doi.org/10.17511/ijmrr.2019.i06.17
1* Raghuram Palaparti, Postgraduate, Department of Cardiology, Osmania General Hospital, Hyderabad, Telangana, India.
2 Imamuddin Syed, Professor, Department of Cardiology, Osmania General Hospital, Hyderabad, Telangana, India.
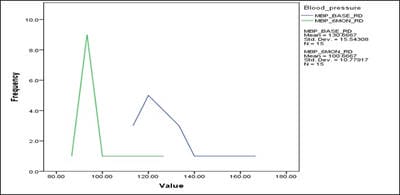
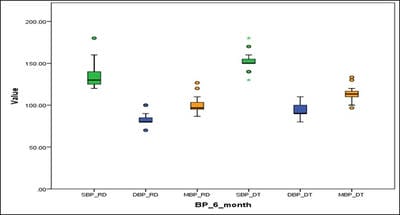
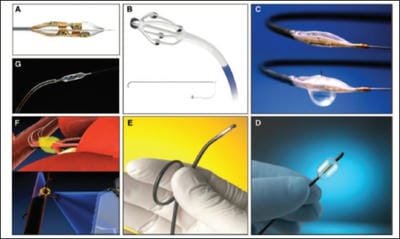
Introduction: Catheter-based renal denervation selectively reduces renal sympathetic efferent activity and is accompanied by an increase in renal blood flow and reduction in plasma renin activity. Thus, ablation of afferent and efferent renal nerves in patients with treatment-resistant hypertension probably leads to reductions in blood pressure. Material and methods: The present study conducted a non-randomized case-control study and enrolled 15 patients who underwent renal denervation therapy for resistant hypertension as cases and 16 patients who were on medical management for resistant hypertension served as controls. Results: It was found that catheter based renal denervation is safe, significantly reduces blood pressure at 1 month, 3 months and 6 months of follow-up without any major adverse events. It was observed that a significant BP reduction when compared to patients only on medical therapy. The mean number of drugs decreased significantly in the denervation group in follow-up. Conclusions: Though the present study showed a significant BP reduction in patients with renal denervation, a significant effect on BP was not observed in a large randomized trial simplicity HTN-3 and major criticism was on the trials design and neuroscience failings. Even today the clinical dilemma is still continuing and further evaluation in rigorously designed clinical trials are necessary to validate alternative methods of renal denervation or to confirm previously reported benefits of renal denervation. The current study anticipate that future trials will also address the effectiveness of renal denervation in disease states other than hypertension.
Keywords: Comparison, Medical therapy, Renal denervation, Resistant hypertension
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Postgraduate, Department of Cardiology, Osmania General Hospital, Hyderabad, Telangana, India. Email: |
Palaparti R, Syed I. Comparison of medical therapy with renal denervation in patients with resistant hypertension. Int J Med Res Rev. 2019;7(6):559-567. Available From https://ijmrr.medresearch.in/index.php/ijmrr/article/view/1116 |


 ©
©