Trisomy 13 mosaicism syndrome with atypical plurimalformative phenotype
Albu C.1*, Albu D.2, Albu S.3
DOI: https://doi.org/10.17511/ijmrr.2019.i06.19
1* Cristina-Crenguta Albu, Lecturer, Department of Genetics, University of Medicine and Pharmacy “Carol Davila”, Bucharest, Romania.
2 Dinu-Florin Albu, Associate Professor, Department of Obstetrics and Gynecology, University of Medicine and Pharmacy “Carol Davila”, Bucharest, Romania.
3 Stefan-Dimitrie Albu, DMD, Alco San Medical Center, Bucharest, Romania.
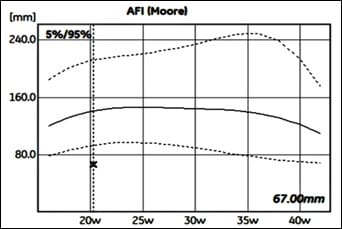
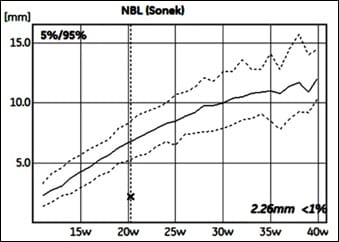
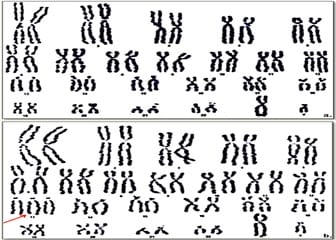
Introduction: Orofacial clefts are important congenital malformations of the lip, palate, or both caused by complex genetic and environmental factors. Aims and Objectives: The present study aims to highlight the phenotypic heterogeneity of trisomy 13 mosaicism. Material and Methods: We present one clinical case of a 30-year-old, Caucasian woman who is pregnant for the first time. Techniques of work study: anamnesis, clinical examination, serological tests for Toxoplasmosis, Rubeola, CMV and Herpes, ultrasound examination at 20 weeks gestation with General Electric Echographe Voluson E10 BT18, amniocentesis, fetal chromosome analysis and genetic counseling. Results: Ultrasound examination showed a viable singleton fetus with intra-uterine growth restriction, oligohydramnios, bilateral cleft lip and cleft palate, hypoplastic nasal bone and bilateral polycystic kidneys. Amniocentesis was done, and the fetal chromosomal analysis revealed a fetus with 46, XY/47, XY,+13 mosaic karyotype. After a complex genetic counselling the parents opted, to terminate the pregnancy. The autopsy confirm the prenatal ultrasound diagnosis. Conclusion: Routine ultrasound examination during pregnancy and specific genetic testing are essential for the early prenatal detection of major structural fetal anomalies associated with rare genetic chromosome syndromes.
Keywords: Oligohydramnios, Cleft lip/palate, Polycystic kidneys, Ultrasound diagnosis, Trisomy 13 mosaicism, Prenatal testing, Genetic counseling
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Lecturer, Department of Genetics, University of Medicine and Pharmacy “Carol Davila”, Bucharest, Romania. Email: |
Albu CC, Albu DF, Albu SD. Trisomy 13 mosaicism syndrome with atypical plurimalformative phenotype. Int J Med Res Rev. 2019;7(6):574-578. Available From https://ijmrr.medresearch.in/index.php/ijmrr/article/view/1098 |


 ©
©