Prospective study on radiation dose escalation in the treatment of squamous cell carcinoma of oesophagus with definitive concurrent chemo-radiation using three-dimensional conformal radiation therapy
Ashwini L.1, Kumar Kn P.2*, Pavithran K.3, Ragavendra H.4
DOI: https://doi.org/10.17511/ijmrr.2019.i05.02
1 Ashwini L., Radiation Oncologist, Department of Radiation Oncology, Medical Physicist-Amrita Institute of Medical Sciences, Kochi, Kerala, India.
2* Pradeep Kumar Kn, Radiation Oncologist, Department of Radiation Oncology, Srinivasam Cancer Care Multispeciality Hospital, Bangalore, Karnataka, India.
3 Pavithran K., Medical Oncologist, Medical Physicist-Amrita Institute of Medical Sciences, Kochi, Kerala, India.
4 Ragavendra H., Medical Physicist-Amrita Institute of Medical Sciences, Kochi, Kerala, India.
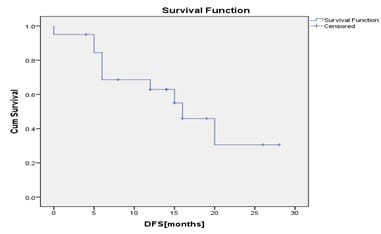
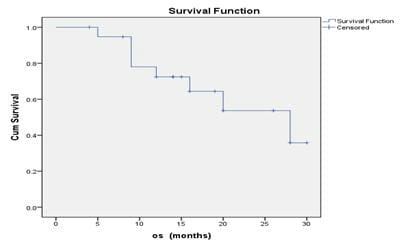
Background: Poor local control and survival rates associated with radiation and chemotherapy in the management of locally advanced carcinoma of oesophagus have encouraged use of radiation dose escalation. This study analysed outcome and tolerance of radiation dose escalation with concurrent chemotherapy in non-metastatic squamous cell carcinoma of oesophagus. Materials and Methods: Patients diagnosed with stage I-III squamous cell carcinoma oesophagus, intended to be treated with radical chemo-radiation, between August 2015 to August 2017 were included in this prospective study. Baseline endoscopy, oral intake score and FACT E-QOL score were documented. Results: Out of total of 20 eligible patients with median age of 64 years, majority had middle thoracic oesophageal tumour (60%), grade 2 dysphagia (75%) on oral intake scale. Patients with tumour length of ≤5cm (55%) or >5cm (45%) were categorised. Majority patients (85%) showed complete response at 3 months post treatment. The oral intake score and quality of life improved in 55% and 85%of the patients, respectively. Ten patients had disease progression with 40% of patients showing disease recurrence. Conclusion: Radiation dose escalation with concurrent chemotherapy in the management of stage I-III, non-metastatic squamous cell carcinoma oesophagus yields a good local control rate at 3 months with less severe complications and improved quality of life.
Keywords: Radiation dose, Squamous cell carcinoma, Oesophagus, Chemo-radiation
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Radiation Oncologist, Department of Radiation Oncology, Srinivasam Cancer Care Multispeciality Hospital, Bangalore, Karnataka, India. Email: |
Ashwini L, Kumar Kn P, Pavithran K, Ragavendra H. Prospective study on radiation dose escalation in the treatment of squamous cell carcinoma of oesophagus with definitive concurrent chemo-radiation using three-dimensional conformal radiation therapy. Int J Med Res Rev. 2019;7(5):348-356. Available From https://ijmrr.medresearch.in/index.php/ijmrr/article/view/1080 |


 ©
©