Evaluation of trans thoracic invasive diagnostic procedures in 50 adult patients of mediastinal diseases
Biswas S.1, Saha R.2, Deb J.3*, Dey P.4
DOI: https://doi.org/10.17511/ijmrr.2019.i04.11
1 Siddhartha Biswas, Department of Respiratory Medicine, N.R.S Medical College, Kolkata, West Bengal, India.
2 Rama Saha, Associate Professor, Department of Pathology, Institute of Post Graduate Medical Education and Research, Kolkata, West Bengal, India.
3* Jaydip Deb, Professor, Department of Respiratory Medicine, N.R.S Medical College, Kolkata, West Bengal, India.
4 Prothoma Dey, Department of Respiratory Medicine, N.R.S Medical College, Kolkata, West Bengal, India.
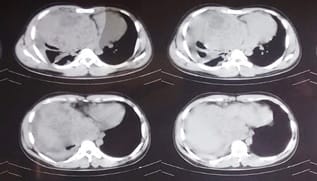
Introduction: Mediastinum is a “Pandora’s box” with many neoplastic and nonneoplastic lesions. Clinico-radiological pattern of mediastinal diseases depends on the size, location and etiology. Hence, non-invasive approach to these cases sometimes leads to diagnostic dilemma. Aims: A prospective study was performed over a 1-year period with the objective of evaluation of diagnostic yields and risk of trans thoracic ultra sound (TTUS) and computed tomography (CT) guided fine‑needle aspiration cytology (FNAC) and Tru-cut biopsy along with comparison of cost-effectiveness among mediastinal diseases where clinical and non-invasive imaging could not conclude the diagnosis. Materials and Methods: A prospective study of mediastinal diseases of the adult population without having any diagnosis admitted in a tertiary care hospital in Eastern India was performed after clearance of the ethical committee of the institute. Fifty cases of mediastinal diseases were seen during the study period. One patient sometimes had undergone more than one procedure. Results: Among 50 patients diagnostic yield of TTUS guided FNA and Tru-cut biopsy were 60% and 63.6% respectively. Diagnostic yield of Thoracic CT guided FNA and Tru-cut biopsy were 85% and 92.3% respectively. As a whole TTUS guided invasive procedure and Thoracic CT guided invasive procedure had a diagnostic yield of 61.5% and 87.9% respectively. Conclusion: Tru-cut biopsy if applicable is much superior to FNAC for a definite diagnosis of the mediastinal diseases. TTUS guided invasive procedures are very much cost-effective and have added advantage of real time guidance and is comparable with CT guided invasive procedures in respect to risk and diagnostic yields.
Keywords: Computed tomography guided invasive procedure, Fine needle aspiration, Mediastinal diseases, transthoracic ultrasound, Tru-cut biopsy, Ultrasound guided invasive procedure
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Professor, Department of Respiratory Medicine, N.R.S Medical College, Kolkata, West Bengal, India. Email: |
Biswas S, Saha R, Deb J, Dey P. Evaluation of trans thoracic invasive diagnostic procedures in 50 adult patients of mediastinal diseases. Int J Med Res Rev. 2019;7(4):324-331. Available From https://ijmrr.medresearch.in/index.php/ijmrr/article/view/1076 |


 ©
©