A clinicopathological study of pleural effusion with special reference to malignant aetiology in a tertiary care hospital in West Bengal
Mandal S.1*, Banik T.2, Barman R.3, Mandal A.4, Kumar Bar P.5
DOI: https://doi.org/10.17511/ijmrr.2019.i04.03
1* Saikat Mandal, Demonstrator, Department of Pathology, Malda Medical College, Malda, West Bengal, India.
2 Tarak Banik, Assistant Professor, Department of Pathology, Malda Medical College, Malda, West Bengal, India.
3 Rina Barman, Assistant Professor, Department of Pathology, Malda Medical College, Malda, West Bengal, India.
4 Animesh Mandal, Assistant Professor, Department of Chest Medicine, Malda Medical College, Malda, West Bengal, India.
5 Prasenjit Kumar Bar, Assistant Professor, Department of Pathology, Malda Medical College, Malda, West Bengal, India.
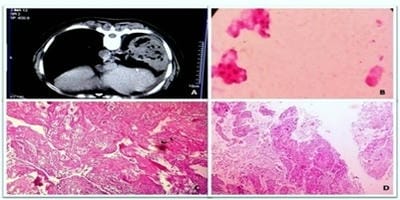
Background: Pleural effusion has varied aetiological factors. It constitutes one of the major causes of morbidity in India as well in other parts of world. Because of the various aetiologies that can cause pleural effusion, itoften present a diagnostic problem, even after extensive investigations. Objective: In this study, authors aimed to identify the common aetiologies causing pleural effusion and their clinical profile in a tertiary care hospital. Materials and Methods: A hospital based cross-sectional study is conducted over a period of one year in tertiary care hospital in West Bengal. 150 patients of pleural effusion above 10 yrs of age were studied. Clinico-pathological, radiological, hematological and biochemical parameters were documented. Results: The most common cause pleural effusion in this study was tuberculosis (64.67%), followed by malignancy (14.67%), parapneumonic effusion (7.33%), cardiac failure (5.33%) and other minor causes. It was commonly seen in male (70%). The occurrence of tubercular pleural effusion was maximum in the age group 31-40 years. Right-sided effusions were more common. Pleural fluid cytology and adenosine deaminase played a pivotal role in the diagnosis of tubercular pleural effusion. Conclusion: The present study highlights tuberculosis as the common causative factor for pleural effusion, labels lung carcinoma as the most common cause of malignant pleural effusion, and defines the clinico-pathological, biochemical and imaging characteristics of different aetiologies of pleural effusion.
Keywords: Pleural effusion, Tubercular effusion, Malignant effusion
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Demonstrator, Department of Pathology, Malda Medical College, Malda, West Bengal, India. Email: |
Mandal S, Banik T, Barman R, Mandal A, Bar PK. A clinicopathological study of pleural effusion with special reference to malignant aetiology in a tertiary care hospital in West Bengal. Int J Med Res Rev. 2019;7(4):266-272. Available From https://ijmrr.medresearch.in/index.php/ijmrr/article/view/1068 |


 ©
©