Predictive accuracy of CURB-65 as comparedto PSI scorein the severity assessment of community acquired pneumonia
Praveen G.S.1, Fathahudeen. A.2*, S. Nair R.3, Kumari K A.4, Nair S.5, Moosan H.6, Vishnu R.7
DOI: https://doi.org/10.17511/ijmrr.2019.i03.06
1 Praveen G.S, Department of Pulmonary Medicine, Govt Medical College, Thiruvananthapuram, Kerala, India.
2* Fathahudeen. A, Department of Pulmonary Medicine, Govt Medical College, Ernakulam, Kerala, India.
3 Reshmi S. Nair, Department of Pulmonary Medicine, Govt Medical College, Thiruvananthapuram, Kerala, India.
4 Anitha Kumari K, Department of Pulmonary Medicine, Govt Medical College, Thiruvananthapuram, Kerala, India.
5 Sanjeev Nair, Department of Pulmonary Medicine, Govt Medical College, Thiruvananthapuram, Kerala, India.
6 Hisham Moosan, Achutha Menon Centre for Health Sciences and Technology, Thiruvananthapuram, Kerala, India.
7 Vishnu R, Department of Radiodiagnosis, Govt Medical College, Thiruvananthapuram, Kerala, India.
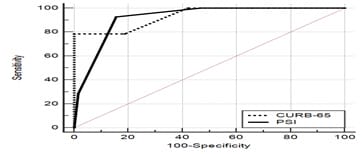
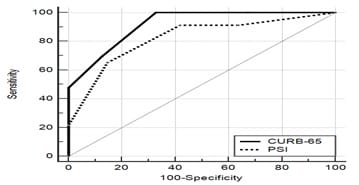
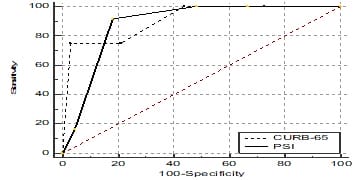
Introduction: Pneumonia Severity Index (PSI) and CURB-65 rule for community acquired pneumonia (CAP) have been developed to stratify patients based on mortality. Lack of a risk stratifying score like PSI or CURB-65 can lead to significant delay in starting treatment. This study was conducted to find out the ability of CURB-65 score and PSI to predict clinically relevant outcomes. Methods: 78 patients diagnosed as CAP admitted to a tertiary care hospital were enrolled into the study. Detailed clinical history was noted and CURB-65 and PSI scores were given with the help of a structured questionnaire in <24 hours of admission. The patients were revisited at day 3 and at discharge and data collected. Results:Out of 78 patients included in the study, 60 were males and 18 were females. Of the 78 patients, 14 died accounting for aninhospital mortality of 17.94%. Mortality in the mild, moderate and severe groups of CURB-65 were 0%, 16.7% and 47.8% respectively. Mortality in the mild, moderate and severe groups of PSI were 1.8%, 50% and 80% respectively. Area under the curve (AUC) for CURB-65 and PSI in terms of in hospital mortality were 0.935 and 0.920 respectively. Conclusion: The CURB-65 and PSI scores correlated well with mortality and other severity indicators. The CURB-65 has a better discriminatory power than PSI inour study. Because of its simplicity in addition to its better discriminatory power than PSI, CURB-65 may be better suited as a severity scoring system in CAP.
Keywords: CAP, CURB-65, in-hospital mortality, PSI
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Department of Pulmonary Medicine, Govt Medical College, Ernakulam, Kerala, India. Email: |
Praveen GS, Fathahudeen A, Nair RS, Kumari K A, Nair S, Moosan H, Vishnu R. Predictive accuracy of CURB-65 as comparedto PSI scorein the severity assessment of community acquired pneumonia. Int J Med Res Rev. 2019;7(3):182-189. Available From https://ijmrr.medresearch.in/index.php/ijmrr/article/view/1056 |


 ©
©