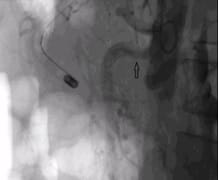
Endovascular Management of Acute Superior Mesenteric Artery Thrombosis in a Delayed Setting
Saxena A.1*, Srivastava P.2
DOI: https://doi.org/10.17511/ijmrr.2019.i02.10
1* Agamya Saxena, Noble Hospital, Bhopal, Madhya Pradesh, India.
2 Prashant Srivastava, Noble Hospital, Bhopal, Madhya Pradesh, India.
Acute mesenteric ischemia [AMI] is a life-threatening situation, the diagnosis of which is often missed in early stages. Late diagnosis often precludes endovascular management as the primary treatment. The authors here present a case of seven days history of acute mesenteric ischemia in a young female, who not just benefited from endovascular management, but also a major surgical intervention was avoided and was discharged from the hospital uneventfully. The decision to consider a patient for endovascular management in a late stage, requires a good interdisciplinary communication and successful outcome in such a scenario is rarely achieved.
Keywords: Acute mesenteric ischemia, Thrombosis, Acute Superior Mesenteric Artery
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Noble Hospital, Bhopal, Madhya Pradesh, India. Email: |
Saxena A, Srivastava P. Endovascular Management of Acute Superior Mesenteric Artery Thrombosis in a Delayed Setting. Int J Med Res Rev. 2019;7(2):112-114. Available From https://ijmrr.medresearch.in/index.php/ijmrr/article/view/1049 |


 ©
©