A case of lateral medullary syndrome with unilateral selective thermoanaesthesia
Mujeeb V.1, Tyagi A.2*, Jambunathan P.3
DOI: https://doi.org/10.17511/ijmrr.2019.i01.09
1 V.R. Mujeeb, Senior Advisor, Department of Medicine and Gastroenterology, Command Hospital, Pune, Maharastra, India.
2* Arun Tyagi, Professor & HOD, Department of Medicine, DVVPF’s Medical College, Ahmed Nagar, Maharashtra, India.
3 Prashant Jambunathan, Graded Specialist, Department of Medicine, Armed Forces Medical College, Pune, Maharashtra, India.
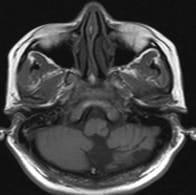
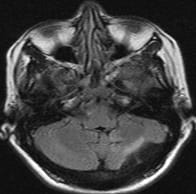
A 42-year-old female was admitted to tertiary care teaching hospital with history of headache, vertigo, difficulty in swallowing both liquids and solids, vomiting, gait ataxia, drooping of left eyelid, inability to feel hot and cold on right side of body and diplopia of forty-fivedays’ duration. Clinical examination and neuroimaging were suggestive a posterior circulation stroke, with lateral medullary syndrome.The patient had selective thermoanaesthesia on the right side, including the face, which is an atypical finding, given the clinical setting.
Keywords: Stroke, CVA, Lateral medullary syndrome, Hypoplasia, Vertebral, Thermoanaesthesia
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Professor & HOD, Department of Medicine, DVVPF’s Medical College, Ahmed Nagar, Maharashtra, India. Email: |
Mujeeb VR, Tyagi A, Jambunathan P. A case of lateral medullary syndrome with unilateral selective thermoanaesthesia. Int J Med Res Rev. 2019;7(1):50-53. Available From https://ijmrr.medresearch.in/index.php/ijmrr/article/view/1035 |


 ©
©