Prognostic significance of primary tumour volume in nasopharyngeal carcinoma – a single institute study
Shamsundar S.1, Jagannath K.P.2*, Niveditha S.3, Aradhana K.4, Nanda R.5, Thejaswini B.6
DOI: https://doi.org/10.17511/ijmrr.2019.i01.05
1 S.D. Shamsundar, Assistant Professor, Department of Radiation Oncology, Kidwai Memorial Institute of Oncology, Bangalore, Karnataka, India.
2* Jagannath K.P., Associate Professor, Department of Radiation Oncology, Kidwai Memorial Institute of Oncology, Bangalore, Karnataka, India.
3 Niveditha S., Resident, Department of Radiation Oncology, Kidwai Memorial Institute of Oncology, Bangalore, Karnataka, India.
4 K. Aradhana, Associate Professor, Department of Radiation Oncology, Kidwai Memorial Institute of Oncology, Bangalore, Karnataka, India.
5 R. Nanda, Associate Professor, Department of Radiation Oncology, Kidwai Memorial Institute of Oncology, Bangalore, Karnataka, India.
6 B. Thejaswini, Professor, Department of Radiation Oncology, Kidwai Memorial Institute of Oncology, Bangalore, Karnataka, India.
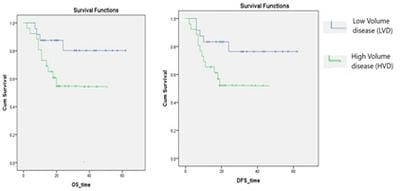
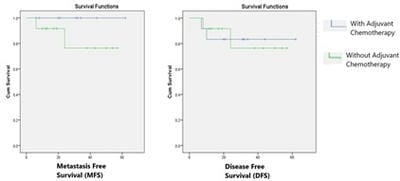
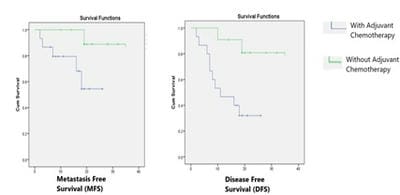
Introduction: Nasopharyngeal carcinoma is very uncommon in the southern part of India, the age-adjusted incidence rate is less than 1 per 1,00,000 population. This study is undertaken to evaluate the outcome of nasopharyngeal carcinoma and its correlation with Primary tumor volume. Material and methods: Total of 50 non-metastatic nasopharyngeal carcinoma patients treated with concurrent chemo radiation between January 2013 and December 2015 were included in the study. All patients were treated via IMRT with dose of 66-70Gy, along with concurrent chemotherapy. Results: The median follow up for the group was 24 months. The median Gross tumor volume of primary disease and nodal disease was 61.6 cubic centimetres and 35.4 cubic centimeters respectively. The 2 year Disease free survival and Overall survival for the entire group was 64% and 68% respectively. There was significant difference (p-0.018) between disease free survival of low volume disease group (LVD) which was 78 % as compared to high volume disease (HVD) group 52% at 24 months, similarly Overall survival was also significantly better (p-0.015) in LVD group as compared to HVD group 80% vs 55% at 24 months. Conclusion: Our patients had large volume primary disease, the OS and DFS was significantly better in LVD patients, adjuvant chemotherapy after concurrent chemoradiotherapy had no additional benefit for LVD patients but improved DFS and MFS in HVD Patients.
Keywords: Nasopharyngeal Carcinoma, Tumour volume, Prognostic factor
| Corresponding Author | How to Cite this Article | To Browse |
|---|---|---|
| , Associate Professor, Department of Radiation Oncology, Kidwai Memorial Institute of Oncology, Bangalore, Karnataka, India. Email: |
Shamsundar SD, Jagannath KP, Niveditha S, Aradhana K, Nanda R, Thejaswini B. Prognostic significance of primary tumour volume in nasopharyngeal carcinoma – a single institute study. Int J Med Res Rev. 2019;7(1):24-29. Available From https://ijmrr.medresearch.in/index.php/ijmrr/article/view/1031 |


 ©
©